-
PDF
- Split View
-
Views
-
Cite
Cite
Stylianos Kapetanakis, Danai Chourmouzi, Grigorios Gkasdaris, Vasileios Katsaridis, Eleftherios Eleftheriadis, Panagiotis Givissis, A rare case of spinal cord compression due to cervical spine metastases from paraganglioma of the jugular foramen—how should it be treated?, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy005, https://doi.org/10.1093/jscr/rjy005
Close - Share Icon Share
Abstract
Paragangliomas are benign neoplasms that arise from the autonomic nervous system and the associated paraganglia. Although benign, they have been shown to possess metastatic potential. Involvement of the spine is rare. Even rarer is considered the involvement of the cervical spine. We report a case of a patient with a history of an extra-adrenal non-functional paraganglioma of the jugular foramen which was initially treated with intra-arterial embolization. After a 3-year disease-free follow-up, the patient was presented with symptoms of spinal cord compression due to spinal metastases in C2 and C3 vertebrae. The patient was then treated with surgical decompression and external beam radiation. Therapeutic management with additional treatment options is now under discussion by a multidisciplinary team. Paraganglioma of the jugular foramen with spinal metastasis is an uncommon presentation where increased physician awareness and long-term follow-up are mandatory for all patients with history of paraganglioma.
INTRODUCTION
Paragangliomas are highly vascular neuroendocrine tumors that arise from chromaffin cells of the adrenal medulla (in the case of pheochromocytomas) and from neuroendocrine cells of the extra-adrenal autonomic paraganglia. Most paragangliomas are described as benign in nature, but almost 10% have been shown to possess metastatic potential [1, 2]. There have been several reports of metastatic paraganglioma in the literature, but rarely do such tumors metastasize to the spine [3]. In this report, we present a patient with symptoms of spinal cord compression caused by spinal metastases in C2 and C3 vertebra from a primary non-functional extra-adrenal paraganglioma of the jugular foramen. In addition, we review the relevant literature and discuss on the topics of imaging and treatment of this challenging condition.
CASE REPORT
A 52-year-old man presented to our hospital with increasing neck pain and upper extremity weakness. The patient had a history of a right jugular paraganglioma which had been discovered by chance and he had been treated 3 years earlier with intra-arterial embolization. The patient had been found to be disease-free at follow-ups. On computed tomography (CT), a permeative destructive lesion in the right petrous bone arising from the upper portion of the jugular bulb and extending anteriorly to the carotid canal was depicted (Fig. 1A). CT scan and magnetic resonance imaging (MRI) of the patient’s cervical spine showed a destructive mass lesion involving the C2 and C3 vertebral bodies with severe canal stenosis and spinal cord compression. A mottled osteolytic lesion with destruction of C2 and C3 vertebral bodies and involvement of posterior elements was observed (Fig. 1B). MRI showed a hypointense expansile lesion involving the C2 and C3 vertebral bodies with extension into the epidural space compressing the spinal cord. The lesion enhanced homogeneously on post-contrast T1-weighted MR (Fig. 1C–F). Laboratory tests were normal and did not indicate elevated serum normetanephrine/norepinephrine. The patient underwent decompressive surgery with an uncomplicated postoperative course. Histopathological examination revealed an infiltrating neoplasm with tumor cells arranged in solid nests with increased number of mitoses. Tumor cells were positive for chromogranin A. The histologic and immunohistochemical assays were compatible with paraganglioma (Fig. 2). Following his discharge, the patient underwent an outpatient external beam radiation. No family history of paraganglioma was reported.
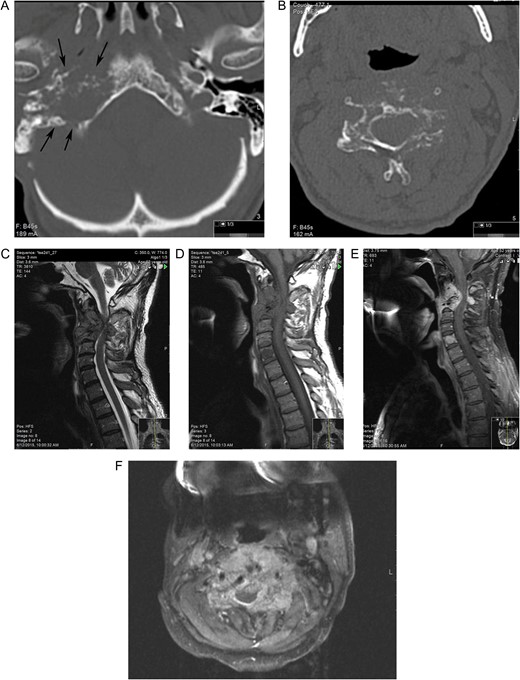
(A) CT shows a destructive lesion in right petrous bone arising at the level of jugular bulb extending anteriorly to the carotid canal (arrow) (B) CT at the level of C3 reveals mottled osteolytic lesion with destruction of the vertebral body and involvement of posterior elements. MRI demonstrates the lesion to be hypointense on sagittal T1-weighted image (C) isointense on T2-weighted (D) and with avid enhancement on post-contrast sagittal (E) and axial (F) TI fat-sat images and epidural extension of the tumor with spinal cord compression. Note avid enhancement of the metastatic lesion of C5 vertebrae body as well.
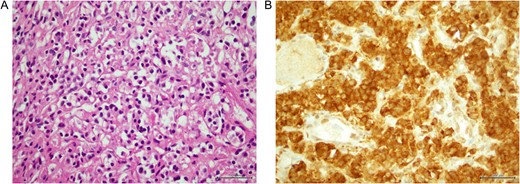
(A) Osteolytic invasion by paraganglioma (B) tumor cells expressing chromogranin A.
DISCUSSION
Generally, paragangliomas account for only about 0.3% of all neoplasms [4]. Most paragangliomas are described as benign in nature, but almost 10% have been shown to possess metastatic potential [2]. Usually, paragangliomas are seen within the adrenal medulla giving rise to pheochromocytoma and only 10% arise outside the adrenal glands. In the head and neck region, the carotid body is the most common site of occurrence followed in frequency by the jugulotympanic and vagal paragaglioma [5].
Malignant paraganglioma is considered a rare presentation, since in most cases the mass is asymptomatic and slow-growing. Its malignancy is diagnosed by local recurrence after resection of the primary mass, or findings of distant metastases. Vertebral metastases are rare and even rarer are considered the cervical metastases [4]. In our case, the paraganglioma was non-functional without any symptomatology of paroxysmal hypertension, palpitation, headache or sweating. It became symptomatic, due to mechanical compression of the spinal cord, when it metastasized to the cervical spine.
Awareness of imaging manifestations of spinal metastatic disease is essential for both the diagnosis and the follow-up. Bone scintigraphy has been the standard initial imaging method for screening of skeletal metastases. CT scans can recognize a bony metastatic lesion earlier than an X-ray. Both bony involvement and neural compression from epidural tumor are demonstrable by MRI, however, MRI cannot distinguish this lesion from other spinal tumors [4, 6]. Thus the diagnosis is confirmed on the histology and immunohistochemical analysis of the intraoperative tissue [4]. In our report, the presence of an infiltrating mass with tumor cells arranged in solid nests, osteolytic invasion, increased number of mitoses and tumor cells positive for chromogranin A confirmed the diagnosis.
Regarding the primary site, the combined therapeutic approach with preoperative selective embolization followed by surgical resection is the safest and most effective method for complete excision of tumors with a reduced morbidity rate. Irradiation (gamma knife) is an effective therapy method for residual head and neck paraganglioma [7]. At first, our patient was only treated with intra-arterial embolization without surgical resection. This happened due to the fact that the initial site appeared to be benign and surgically challenging due to its location. The patient remained disease free at the follow-ups.
However, metastases appeared and the therapeutic strategy changed completely. It is believed that the treatment of choice for malignant paragangliomas with vertebral metastasis and cord compression is surgical decompression and adjuvant external beam radiotherapy. Chemotherapy and I131-MIBG have also been used therapeutically in malignant paraganglioma [4]. Our patient underwent decompressive surgery without any complications and outpatient external beam radiation. Treatment with alternative therapies including combination chemotherapy is now under discussion by a multidisciplinary team.
It is challenging to make the appropriate initial choice regarding the management of such cases. Wait-and-see policy may be considered for very slow-growing tumors in patients with multiple medical problems and old age [8]. While the individual behavior of paragangliomas is unpredictable the primary management should be directed towards the complete surgical resection of the primary tumor [9]. The optimal treatment for metastases remains unclear, however, concomitant treatment with radiosurgery and reconstructive surgery have appeared to be both safe and effective [10].
In conclusion, primary paraganglioma of the jugular foramen giving cervical metastases is a very rare and challenging malignant condition. Increased surveillance with clinical assessment and imaging tests is mandatory in the follow-up intervals. Metastatic or not, such cases are challenging to manage and dilemmas may merge regarding the appropriate therapeutic strategy.
CONFLICT OF INTEREST STATEMENT
None declared.
AUTHOR CONTRIBUTIONS
K.S. organized, edited and acted as a guarantor for all aspects of the manuscript. C.D. collected and critically analysed all the radiological findings. G.G. wrote and joined together all aspects of the case forming the main skeleton of the article. K.V. examined the case management and performed the neurosurgical intervention. E.E. performed the gross and histologic evaluation of the pathology specimen. G.P. critically evaluated the whole article and the relevant literature. All the authors have made substantial contributions to conception and design, acquisition of data and data analysis, drafting of the article and critical evaluation, and approval of the version to be published.
REFERENCES
- adrenal glands
- autonomic nervous system
- embolization
- decompression, surgical
- follow-up
- neoplasm metastasis
- paraganglia
- paraganglioma
- patient care team
- spinal cord compression
- spine
- secondary malignant neoplasm of spine
- benign neoplasms
- cervical spine
- vertebrae
- jugular foramen
- interdisciplinary treatment approach



