-
PDF
- Split View
-
Views
-
Cite
Cite
Parthena Deskoulidi, Nektarios Koufopoulos, Pantelis Diamantopoulos, Efthymios Basagiannis, Nikolaos Maltzaris, Thaleia Nikolaidou, Michael Kydonakis, Maria Kotrotsiou, Konstantinos Benetatos, Niki Arnogiannaki, Spiros Stavrianos, Intramuscular granular cell tumor of the gluteal region, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy004, https://doi.org/10.1093/jscr/rjy004
Close - Share Icon Share
Abstract
Granular cell tumors are uncommon, usually benign neoplasms, mainly observed in the head and neck region, chest wall and upper extremities. These tumors account for ~0.5% of all soft-tissue tumors. Less than 2% are malignant. These are associated with poor prognosis. Clinical signs suspicious for malignancy are large size, rapid growth, invasion, recurrence and metastasis. Malignancy is confirmed by histological examination. We present the case of a 79-year-old patient with a 6-month history of a rapidly growing mass in the left gluteal region giving the clinical impression of a malignant tumor. The patient underwent surgical excision of the tumor and the pathology report revealed a granular cell tumor. In difficult cases, multidisciplinary approach is necessary for appropriate diagnosis and management.
INTRODUCTION
Granular cell tumors (GCTs) were firstly described in 1926 by Abrikossoff, although Weber had published one case in 1854 [1]. They are uncommon neoplasms, accounting for ~0.5% of all soft-tissue tumors [2]. The female-to-male ratio is 3:2. GCTs appear to be common in black persons and up to 10% are multiple [3, 4]. Most patients are middle-aged with a peak incidence in the fourth through sixth decades of life. Clinically, they present as asymptomatic, slow-growing solitary nodules, usually smaller than 3 cm. Increased familiar incidence is uncommon, however it has been reported. They were initially named ‘granular cell myoblastomas’ because the origin was assumed to be from skeletal muscles. Various theories have been proposed to explain the origin of GCT, including striated muscles histiocytes and the neural origin from Schwann cells [5]. They may arise in any part of the body, but they have been mainly observed in the head and neck region (tongue, cheek, mucosa and palate), chest wall and upper extremities [6]. GCTs occurring in deep soft tissues are extremely rare, especially those of intramuscular location [7, 8]. Due to rarity, only few studies are present in the literature describing intramuscular GCT, mainly addressing their malignant counterpart. Most GCTs are benign, with some of them displaying local aggressive behavior. Two percent are malignant [9, 10] and associated with poor prognosis. We report a case of GCT showing an uncommon localization in the gluteal region and an unusual clinical behavior.
CASE PRESENTATION
A 79-year-old man was referred to our clinic with a 6-month history of a rapidly growing mass in the left gluteal region. His main complain was pain, radiating down, to the posterior thigh muscles, while in a seated position. He had no previous history of any significant underlying illness, except for gastritis, treated with PPIs and diet. He had also undergone prostatectomy for benign prostatic hyperplasia 2 months before presenting to our clinic. No previous history of trauma in the gluteal or pelvic area was mentioned. At the time of presentation, there was no weight loss, anorexia, fever or other associated symptoms. Physical examination revealed a large, firm, tender mass. Due to rapid growth, the clinical impression was of a malignant neoplasm. Laboratory findings, including lactate dehydrogenase and alkaline phosphatase, were normal. Imaging studies were performed, including pelvic, abdominal and chest computed tomography (CT) and pelvic magnetic resonance imaging (MRI). The CT and MRI examination of the pelvis demonstrated a 7 × 4.4 cm sized soft-tissue mass in the region of left gluteus maximus and gluteus medius muscle. The lesion extended to the surface of the left iliac bone, without infiltrating it (Fig 1). The chest and abdominal CT were performed for detecting metastasis prior to surgery and a CT-guided fine needle aspiration (FNA) biopsy of the mass was performed to determine if the tumor was benign or malignant. The CT was negative for metastasis and the FNA result was inconclusive.
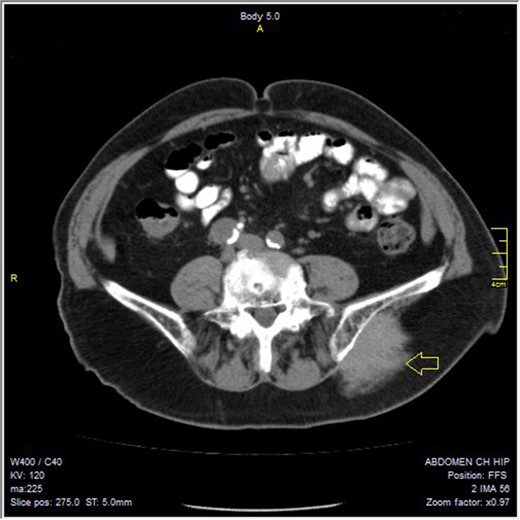

At surgery, an incision was performed parallel to the gluteus maximus muscle. As the tumor remained deep within the gluteus maximus muscle (Fig. 2), a wide excision of a big portion of the underlying gluteus maximus and gluteus medius with a 3–4 cm margin was performed (Figs 3 and 4). Exploration of the sciatic nerve revealed that it was not infiltrated by the tumor.

The wide excision of the portion of the gluteus maximus and medius muscle.

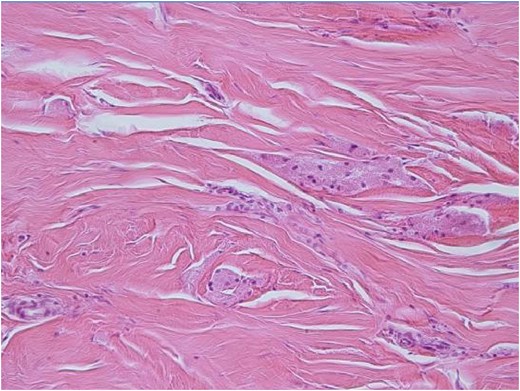
H-E ×200: On medium power examination tumor cells are separated by fine sclerotic collagenous tissue.
On gross examination, the tumor was poorly defined, pale yellow on cut surface with a maximum diameter of 7.6 cm.
Microscopically, the tumor was poorly circumscribed and diffusely infiltrating. Neoplastic cells were large, polygonal with eosinophilic granular cytoplasm and small round to ovoid nuclei. They were separated by sclerotic collagenous tissue (Fig. 5). Few mitotic figures were noticed. Atypia, spindling, high nuclear to cytoplasmic ratio, pleomorphism or areas of necrosis were not identified.
Immunohistochemical study was positive for S-100, CD-68, Inhibin-A, Calretinin, CD-57, NSE and negative for AE-1/AE-3 and Desmin. Ki-67 showed positivity in less than 1% of tumor cells. The tumor was diagnosed as morphologically and immunohistochemically consistent with granular cell tumor.
On postoperative evaluation, 6 months after surgery, there are no signs of recurrence or distant metastasis. The tumor board recommended that the patient was to be closely followed-up, every 6 months, for the following 2 years.
DISCUSSION
GCTs have been reported in a variety of anatomic sites. They are typically located in the dermis or subcutaneous tissue and rarely occur in deep soft-tissue, such as the intramuscular gluteal region. They present as painless masses. Our case is notable due to unusual location, large size and presentation as painful mass. The pain and tenderness were attributed to pressure effects to the sciatic nerve. The differential diagnosis included sarcoma, old hematoma, proliferative myositis and lymphoma. GCTs had not been considered as part of the differential diagnosis. Malignant behavior is rare and is seen in 0.5–2% of the cases [11]. Malignancy can be suggested by clinical findings, such as large size, rapid growth, invasion into adjacent tissue, recurrence and metastasis. The differential diagnosis between benign, atypical and malignant lesions may be very difficult. Fanburg-Smith et al. have proposed the following histological criteria in order to differentiate benign from malignant tumors: necrosis, spindling, vesicular nuclei with large nucleoli, nuclear pleomorphism, high nuclear to cytoplasmic ratio, and increased mitotic activity (>2 mitoses/10 high-power fields). Neoplasms that meet three or more of these criteria are classified as malignant; those displaying only focal pleomorphism but fulfill none of the other criteria are classified as benign, whereas those meeting one or two criteria are classified as atypical. Malignant GCTs are more common in African American women. Patients’ age ranges from 30 to 50 years as in patients in their benign counterpart. Treatment of choice is wide local surgical excision. If resection margins are involved, wider local excision may be recommended to decrease the risk of recurrence, which occurs in 21–50% of GCT cases [12]. In our case, the tumor was completely excised with free margins. Other adjunctive treatment, such as chemotherapy and radiation were considered. However, the surgical excision was very successful and the malignant potential of the tumor was low. Therefore, no other treatments were considered necessary (patients’ age and general condition were also taken into account).
In conclusion, GCTs should be considered in the differential diagnosis of a rapidly growing intramuscular tumors. Multidisciplinary approach (oncology tumor board, pathologist, radiologist, surgeon) is necessary for proper diagnosis, treatment and follow-up.
CONFLICT OF INTEREST STATEMENT
None declared.



