-
PDF
- Split View
-
Views
-
Cite
Cite
Athanasios Syllaios, Dimitra Daskalopoulou, Nikolaos Bourganos, Anastasia Papakonstantinou, Evangelia Triantafyllou, Antonios Koutras, Christos Georgiou, Giant colonic diverticulum—a rare cause of acute abdomen, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy009, https://doi.org/10.1093/jscr/rjy009
Close - Share Icon Share
Abstract
Giant colonic diverticulum (GCD), defined as diverticulum larger than 4 cm, is a rare entity. It is generally a manifestation of colonic diverticular disease and can have dramatic complications such as perforation, abscess, volvulus, infarction and adenocarcinoma. This report documents the case of a 63-year-old man coming to the Emergency Department with acute abdomen due to a perforation of a GCD. In the plain abdominal X-ray the ‘Balloon-sign’ was revealed, computed tomography scan and Hartmann’s procedure were performed. Acute abdomen can occur as a manifestation of a complication of a GCD, and this report highlights the fact that GCD should be considered for patients with a high risk of diverticular disease and abdominal pain.
INTRODUCTION
Giant colonic diverticulum (GCD) is defined as a diverticulum larger than 4 cm in diameter. It is an uncommon condition with <200 studies described in the current literature. Acute abdomen has been reported in 6% of the cases, while perforation can occur at presentation or at the time of surgery in 26.5% of the cases. Volvulus, colonic obstruction, infarction and adenocarcinoma constitute less common complications of the GCD [1]. Our main objective is to present this rare entity as potential cause in the differential diagnosis of acute abdomen, particularly among patients aged 60 or older.
CASE REPORT
A 63-year-old man was referred to the surgical emergency department because of severe abdominal pain, fever and abdominal distention. The patient complained of abdominal pain during defecation for about a week, as well as abdominal swelling and a sensation of weight during urination for 1 month. His medical history was unremarkable and he had never undergone a colonoscopy. The physical examination showed tenderness and rigidity in the left iliac fossa.
A plain abdominal X-ray presented a solitary, air-filled structure with smooth margins in the lower abdomen, while a chest X-ray revealed the presence of free air in the abdominal cavity (Fig. 1a). An abdominal computed tomography (CT) scan showed a large, 9 × 9.5 cm2, thin-walled, cyst-like lesion with air-fluid level adherent to the sigmoid colon as shown in Fig. 1b.
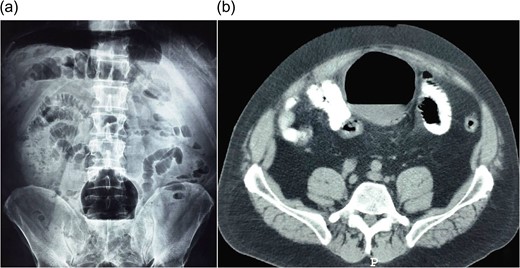
(a) Abdominal X-ray shows an air-filled structure in the lower abdomen (Balloon-sign). (b) Abdominal CT scan shows an air-filled cavity associated with the colon.
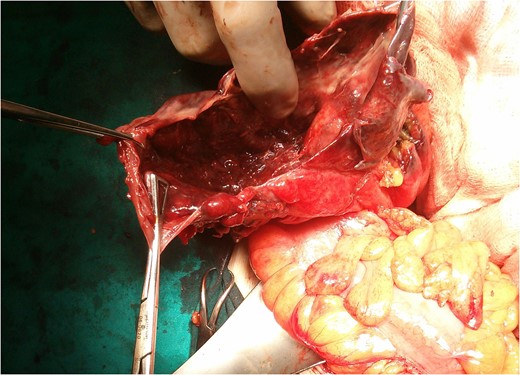
At exploratory laparotomy, a large cystic mass was found adherent to the sigmoid colon (Fig. 2) and Hartmann’s procedure was performed. The resected specimen of the GCD and sigmoid colon is shown in Fig. 3. The postoperative recovery was uneventful and the patient was discharged on postoperative Day 7.
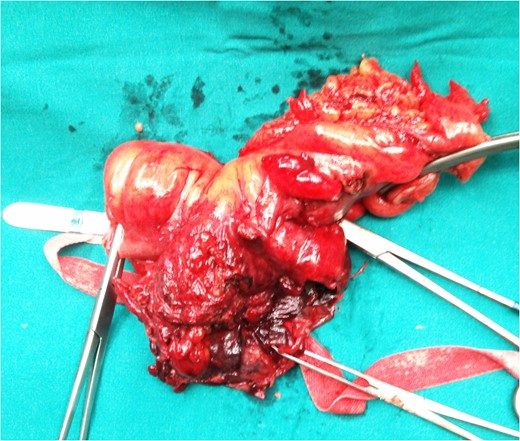
Resected specimen of the giant colonic diverticulum and sigmoid colon.
Pathological assessment of the specimen showed diverticulosis and a 8 × 7 × 6.8 cm3 ruptured diverticulum with extensive acute inflammation of serosal tissue, fibrous tissue and foreign-body giant cell reaction around fecal matter. A colorectal polyp with sites of tubular adenoma with focal high-grade dysplasia distal of the GCD was revealed.
In accordance with the classification suggested by McNutt et al., the features of the specimen were consistent with type II GCD. Colostomy reversal was performed 4 months later.
DISCUSSION
Diverticular disease is a common manifestation with high prevalence among individuals older than 60 years in the western world.
GCD is a rare condition occurring in the sigmoid colon in more than 90% of the cases, that was initially described in 1946 by Bonvin and Bonte. Concomitant diverticular disease is present in 85% of the patients. Although age at diagnosis ranges from 32 to 90 years, most cases have been described after the age of 60 [1]. In most reported cases of GCD, the diameter ranges between 4 and 9 cm, yet diverticula as large as 40 cm have been described [2].
McNutt et al. classified GCD in three distinct subtypes. Type I is a pseudodiverticulum containing remnants of muscularis mucosa or muscularis propria and gradually increasing in size (22%). Type II is an inflammatory diverticulum without any intestinal layers, which is secondary to a local perforation of the mucosa and submucosa, creating an abscess cavity that communicates intermittently with the bowel lumen. The particular type of diverticulum contains fibrous scar tissue (66%). Type III is a true diverticulum consisting of all the layers of the bowel (12%) [1].
There are two main hypotheses to the pathogenesis of the GCD. The first claims that an unidirectional ball-valve mechanism, through a tiny communicating diverticular neck causes air entrapment and gradual enlargement of the diverticulum [3], while the other asserts that gas forming organisms are responsible for GCD [1].
The clinical presentation of GCD can be variable. One-third of the patients present with chronic symptoms, such as abdominal pain, distention and altered bowel habits. Approximately 10% of the cases are asymptomatic, as an abdominal mass constitutes an incidental finding. An acute presentation (30–35%) involves the occurrence of acute abdominal pain associated with fever, vomiting and rectal bleeding. Complications of the GCD are reported in 15–35% of the cases. Patients may have an acute abdomen (6%) due to perforation or other less common complications such as abscess, volvulus and infarction [1]. Adenocarcinoma within or distal to the GCD has been reported in 2% of the cases [4].
Abdominal X-ray and CT scan are the investigations of choice for diagnosing GCD. A large, smoothly marginated, air-filled cyst (‘Balloon-sign’) with or without air-fluid level is revealed on the abdominal X-ray [5]. An abdominal CT scan shows an air-filled cavity associated with the colon. Barium enema can demonstrate the communication with the bowel lumen in 60–70% of the cases. However, perforation may occur as a complication [6].
Resection of the diverticulum and adjacent colon with primary anastomosis, with or without a temporary diverting ileostomy, is the recommended treatment for uncomplicated GCD [7], while a laparoscopic approach may be feasible in some patients [8]. In the setting of complications, Hartmann’s procedure might be performed [1].
In conclusion, acute abdomen can occur as a manifestation of a complication of GCD such as perforation. Hence, we suggest that the particular condition should be considered for patients with a high risk for diverticular disease. Plain abdomen X-ray and CT scan contribute to the diagnosis. Resection of the diverticulum and the adjacent colon is preferred as treatment of choice.
CONFLICT OF INTEREST STATEMENT
None declared.



