-
PDF
- Split View
-
Views
-
Cite
Cite
Ravi Maharaj, Barry Raghunanan, Wayne Mohammed, Rakesh Rambally, Vandana Devika Sookdeo, Dave Harnanan, Wayne A Warner, A rare case of massive lower gastrointestinal bleeding from a ruptured splenic artery aneurysm, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy003, https://doi.org/10.1093/jscr/rjy003
Close - Share Icon Share
Abstract
Splenic artery aneurysms (SAAs) are an extremely rare cause of asymptomatic massive lower gastrointestinal bleeding with less than a handful of patients surviving such a presentation. A 24-year-old female presented in shock after multiple episodes of massive rectal bleeding. Imaging revealed a heterogeneous mass arising from the tail of the pancreas eroding into the splenic flexure of the colon. Further episodes of bleeding led to an exploratory laparotomy. Intraoperatively, a suspected neoplastic process arising from the tail of the pancreas with contiguous involvement of the splenic flexure of the colon and the greater curvature of the stomach was noted. Distal pancreaticosplenectomy, gastric wedge resection with segmental colectomy and primary anastomosis were performed. Histology revealed a SAA with rupture into the colon. This case report shows that en-bloc resection of a ruptured SAA can be performed with success in the emergency setting.
INTRODUCTION
Splenic artery aneurysms (SAAs) are the third most common intra-abdominal aneurysm after those of the aortic and iliac artery [1]. The female to male ratio is 4:1 with rupture occurring more frequently in men [2]. They are mostly asymptomatic, with occasional symptoms such as left upper quadrant/epigastric pain, hypovolemic shock and bleeding from the gastrointestinal tract arising in about 5% of patients [3].
We describe the case of a 24-year-old female of African ancestry who presented with a SAA. This case highlights the risk factors, radiologic and intraoperative findings, histologic diagnosis and surveillance of a SAA patient in the setting of a developing country.
CASE REPORT
A 24-year-old Trinidad and Tobago female national of African ancestry, without any known co-morbidities, presented to the emergency department with a 1-day history of massive rectal bleeding accompanied by dark red clots. En route to the hospital, she suffered a catastrophic bleed and upon arrival was in shock with complaints of mild abdominal pain, syncope and severe lethargy.
On examination, the patient was somewhat alert and oriented. Presenting vitals reflected class III hypotensive shock which responded adequately to aggressive fluid resuscitation. Hourly urine output was adequate and the nasogastric tube aspirate and free drainage were blood free. Her abdomen was soft with mild epigastric tenderness but no signs of perotinism. An ill-defined, supraumbilical fullness was noted and dark red blood and stool appeared on digital rectal exam. Biochemical assessments, electrocardiogram, abdominal and chest X-rays were all unremarkable. A pregnancy test was negative.
A triphasic, contrast enhanced computed tomography (CT) scan revealed a 6 cm × 5.2 cm well defined, heterogeneous, hypodense mass arising from the pancreatic tail, with an extremely enhancing component (200 Hounsfield units) on its lateral side, a feeder vessel arising from the splenic artery and a small splenic infarct (Fig. 1). Fascial margins of the mass were poorly defined from the splenic hilum and splenic flexure of the large intestine (Fig. 2). CT imaging was supportive of a differential diagnosis of a solid pseudopapillary tumor of the tail of the pancreas with invasion of the colonic wall and compression of the stomach.

CT image showing the ‘ying yang’ sign of the SAA. White arrow shows the origin from the splenic artery. Black arrow shows a splenic infarct.
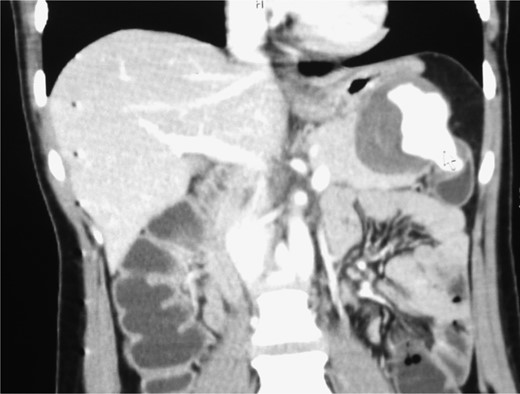
CT shows the point of communication (free rupture) between the aneurysm and splenic flexure of the colon.
Once stable, the patient was counseled about possible interventions. Eight hours post-admission, after transfusion with two units of packed red blood cells, her vitals remained stable, adequate hourly urine output resumed and the bleeding abated. However an hour later, she had an enormous episode of rectal bleeding losing ~1.5 L of blood. She became acutely unresponsive and unstable and was rushed to the operating room while being resuscitated with crystalloids, colloids and uncross-matched blood.
An exploratory laparotomy revealed the presence of blood in the distal ileum and large bowel. Further dissection uncovered a mass adherent to the posterior stomach that arose from middle and distal pancreas and involved the distal transverse colon. With a differential diagnosis of cancer and with consult by the operating team, the decision for definitive surgery was made. An en-bloc resection of the mass, distal pancreatectomy and splenectomy, resection of the cuff of the distal transverse colon and a wedge resection of stomach were performed.
Histopathology confirmed the specimen to a SAA, with a 1 cm rupture through the colonic wall (Fig. 3A and B). On microscopic examination, the wall of the colon showed attenuation and loss of the muscle layers with bleeding into the lumen of the colon (Figs 4 and 5).
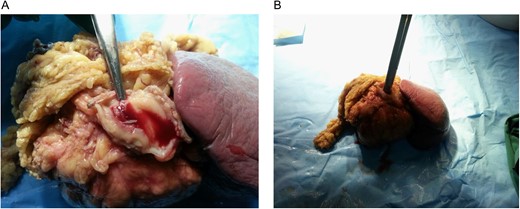
En-bloc specimen. (A) Hemorrhage into the colonic lumen from the aneurysmal communication. (B) The specimen showing free rupture of the aneurysm into the colonic lumen.
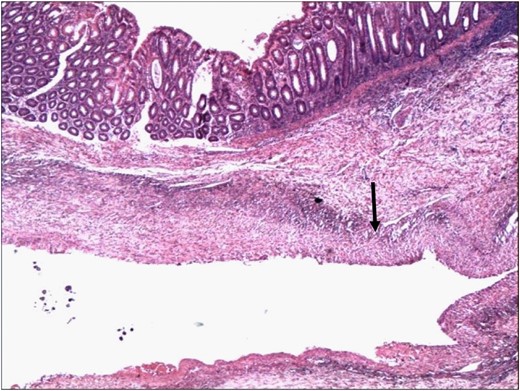
Wall of the colon showing attenuation and loss of the muscle layers. The wall of the aneurysm is indicated by the arrowhead (H&E 4×).
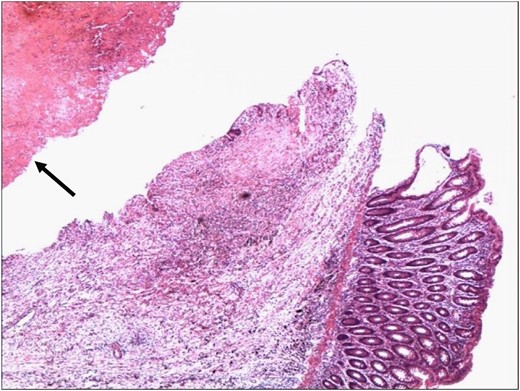
Point of rupture of the aneurysm into the lumen of the colon. The lumen of the aneurysm contains blood clot (arrowhead) (H&E 4×).
The patient remained stable throughout the surgery and her post-operative period. The patient was asymptomatic 2 years post-surgery.
An exhaustive search of the PubMed/Medline and EMBASE medical databases from inception (1946–present) was performed. The search strategy was ‘(developing countries, Latin America, Trinidad and Tobago and Caribbean) AND (‘splenic artery’ OR ‘spleen artery aneurysm’) AND ‘ruptured aneurysm’’. No citations were found after limiting final retrieval to English language, humans and case reports. To the best of our knowledge, this is the first case report of a SAA in the Caribbean and Latin America.
DISCUSSION
The prevalence of SAA is low [4], and pelvic rectal bleed secondary to SAA is extremely rare (<10 reported cases) [5]. While patients can present with SAA at any age it is much more commonly observed in patients 50–60 years. Our patient presentation at 24 years is extremely rare. While the etiology is often unknown it has been associated with a myriad of systemic diseases including hypertension, cirrhosis, arteritis and collagen vascular disease. Interestingly, our patient did not have a history of these conditions.
CT angiography diagnostic regimen is a powerful minimally invasive technique for the evaluation of blood vessel disease and related conditions, such as aneurysms or blockages. Catheter directed angiography as a diagnostic tool for massive lower gastrointestinal bleeding (GI) bleeds is also widely used in conjunction with angiographic coiling and a stent for immediate therapeutic relief. In most developing countries, endovascular management approaches, including availability of endovascular equipment and blood products, for lower GI bleeding are not readily available. In such low-resource environments, emergency patients with massive GI bleeds are managed expectantly. If bleeding persists, open surgical management is the only option.
Treatment for SAA should be undertaken when there is an increased risk of rupture, perforation diameter greater than 2 cm, and in symptomatic, transplant patients and in younger or pregnant women [6]. Those presenting with lower GI represent a distinct entity and management commences with adequate resuscitation and appropriate investigations. Endovascular coil embolization is an attractive first line treatment [5, 7]. However, it is not the preferred clinical approach for the management of giant aneurysms due to suboptimal occlusion of the aneurysm, inflammatory process and increased risk of embolization. Aneurysmectomy, pancreatectomy and splenectomy approaches have been reported [8].
In conclusion, SAAs are an extremely rare cause of lower GI bleeding. Contrast CT for ambiguous cases of lower gastrointestinal bleeding may be warranted, especially in low-resource centers without endoscopy or selective angiography services, to avoid the high-mortality rate associated with undiagnosed lesions.
ACKNOWLEDGEMENTS
The authors acknowledge the assistance of Kim Lipsey, Medical Librarian, Becker Medical Library, Washington University School of Medicine-St. Louis, MO, USA. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the views of the affiliating institutions.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
W.A.W. was supported by Washington University School of Medicine, GSAS/CGFP Fund 94028C.
REFERENCES
- hemorrhage
- heterogeneity
- anastomosis, surgical
- neoplastic processes
- rupture
- shock
- colon
- diagnostic imaging
- histology
- stomach
- survival
- lower gastrointestinal bleeding
- rectal bleeding
- splenic artery aneurysm
- colon resection, partial
- wedge resection
- laparotomy, exploratory
- splenic flexure
- pancreas tail
- pancreaticosplenectomy



