-
PDF
- Split View
-
Views
-
Cite
Cite
Samit Unadkat, Ashok Adams, Polly Richards, Yogesh Bajaj, Paediatric aneurysmal bone cyst: not as easy as ABC, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy008, https://doi.org/10.1093/jscr/rjy008
Close - Share Icon Share
Abstract
Aneurysmal bone cysts (ABCs) are expansile cystic lesions that can affect any bone of the body. Whilst these lesions are histologically benign, the lesions are locally aggressive and can affect the integrity of the affected bone as well as surrounding structures. ABCs arising in the head and neck region, particularly the paranasal sinuses are rare and they are limited to case reports in the literature. Due to the proximity of critical anatomical structures and the visual apparatus, the potential complications can be devastating. The present article discusses both the clinical and radiological findings of an ABC arising from the ethmoid sinuses in a 6-year-old child and the potentially challenging diagnosis with its complex ensuing surgical management. The identification of an ABC arising in the paranasal sinuses is both a diagnostic and surgical challenge and ideally requires complex management in a joint paediatric ENT and craniofacial unit.
INTRODUCTION
Aneurysmal bone cysts (ABCs) are osteolytic bony neoplasms found most commonly in the metaphyses of long bones and vertebrae but exceptionally rarely in the paranasal sinuses. Although regarded as histologically benign, their locally expansile nature poses a threat to the visual apparatus and brain when identified in the paranasal sinuses. The present report illustrates one such case of a primary ABC in a 6-year-old child and the complex subsequent surgical challenges.
CASE REPORT
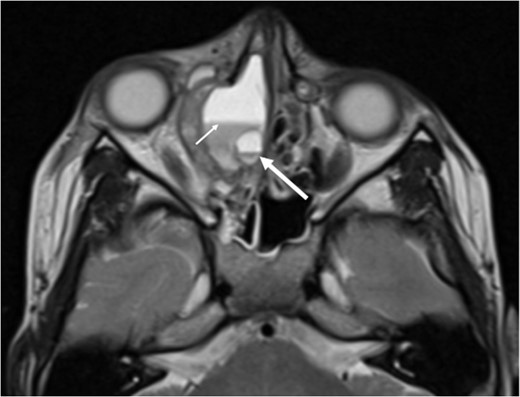
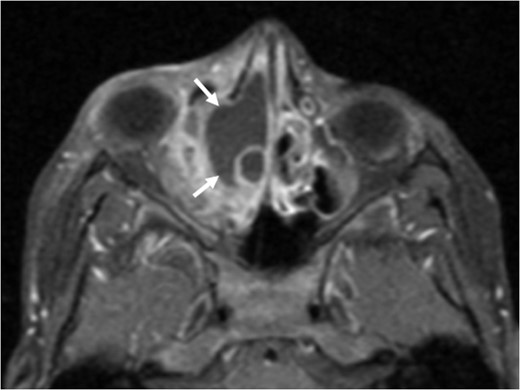
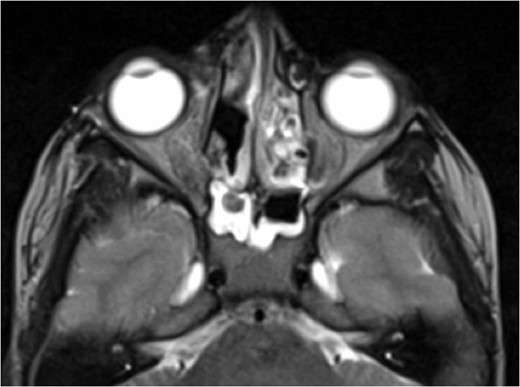
A 6-year-old boy with a background of asthma presented to a tertiary paediatric unit in May 2016 with a 3-day history of right eye pain, proptosis and erythema under the care of the ENT team. A provisional diagnosis of a periorbital cellulitis was made secondary to ethmoid sinusitis and management with intravenous antibiotics (ceftriaxone), intranasal steroids, saline douches and topical oxyxlometazoline was initiated. Ophthalmological assessment demonstrated normal colour vision, acuity and light reflexes bilaterally but also proptosis-related ophthalmoplegia. Computed tomography (CT) imaging of the orbits and paranasal sinuses demonstrated complete opacification of the right-sided paranasal sinuses and compromise of the right frontal and ostiomeatal unit. In addition there was an expansile abnormality centred on the ethmoidal labyrinth with bony remodelling of the lamina papyracea and a subperiosteal collection adjacent to the medial orbital wall (Figs 1 and 2). The most likely diagnosis was felt to be an infective process with mucopyocele formation complicated by a subperisoteal post-septal collection. An MRI scan with gadolinium of the orbits and sinuses confirmed the unilateral pattern of sinus opacification within the right frontal, ethmoids and maxillary sinus. The lesion demonstrated multiple fluid–fluid levels and peripheral enhancement (Figs 3 and 4). The patient was treated by endoscopic drainage of the lesion, which revealed only blood. He initially had some improvement of his proptosis but recurred within a few days and so further, more extensive endoscopic debridement was performed.
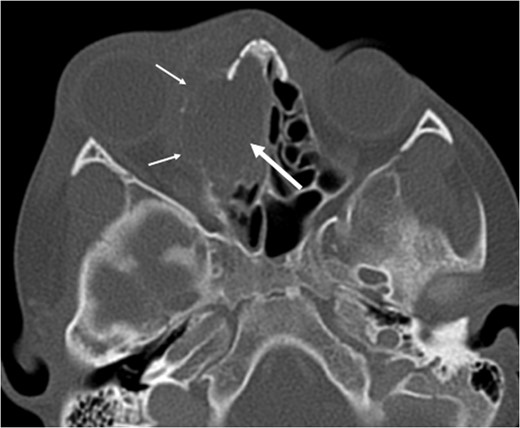
Axial non-contrast CT demonstrating an expansile lesion centred on the right-sided ethmoidal labyrinth (long white arrow) with remodelling of the lamina papyracea (short white arrows).

Axial post-contrast CT demonstrating the peripherally enhancing right-sided intra-orbital subperiosteal component. The expansile lesion centred on the right ethmoidal labyrinth demonstrates a faint fluid–fluid level.
Axial T2 weighted sequence demonstrating the presence of multiple fluid filled levels (short white arrow) within the expansile lesion and smaller cyst present within the larger cyst (long white arrow).
Axial T1 post-contrast sequence with fat suppression demonstrating peripheral enhancement (white arrows) but no internal or solid enhancing components to suggest that this is a secondary ABC.
At this point the MRI was reviewed and the possibility of an ABC was raised. This was due to the presence of fluid–fluid levels, cyst within a cyst appearance and lack of restricted diffusion within the sinonasal contents and material drained at the time of the first endoscopic procedure. He was discharged home on oral co-amoxiclav, and topical betamethasone nose drops.
Unfortunately, in June 2016 his symptoms recurred again, with evidence of soft tissue swelling medial to the medial canthus. Further imaging (CT and MRI) was requested and he was referred to both a quaternary centre for ENT surgery and a bone tumour multidisciplinary team who agreed that the lesion was most likely to represent a primary ABC. In the interim he remained under close evaluation by the ophthalmologists.
He underwent a third surgical procedure in July 2016, this time a joint external and open approach. The histopathology confirmed an ABC and his immediate post-operative was uneventful. His proptosis and ocular motility improved slowly.
Regrettably, the ABC recurred again by October 2016 and the imaging demonstrated substantial erosion of the anterior cranial fossa floor that required a bicoronal and transcranial approach with reconstruction of the medial orbital wall.
Currently (November 2017), he remains well, with near total resolution of the proptosis. His visual acuity is normal and the ophthalmoplegia has resolved. Post-operative imaging has demonstrated good clearance and removal of the cyst (Figs 5 and 6).
Axial T2 weighted sequence following surgical intervention and medial orbital wall reconstruction for the most recent recurrence demonstrating no residual abnormality.

Axial non-contrast CT at the same level demonstrating the resection of the ABC following multiple surgical procedures and a medial orbital wall reconstruction.
DISCUSSION
Aneursymal bone cysts were first described by Jaffe and Lichstenstein [1] and are well known to affect long bones, spine and pelvis. The term arises from their macroscopic description: a cystic, blood-filled cavity within an expanded (aneurysmal) bony wall [2]. Though the pathophysiology of these lesions is poorly understood, ABCs tend to affect long bones, spinal vertebrae and pelvis. They account for 1–2% of all primary bone tumours [3]. Guida et al. [4] report that lesions involving the skull, comprise 3–6% of all ABCs. Very few have ever been reported in the paranasal sinuses and are exceptionally rare in the paediatric population. Most ABCs are considered to represent a primary ABC, however, in up to a third of cases, ABCs are secondary to an underlying lesion (e.g. chondroblastoma) [2].
The diagnosis of an ABC can be challenging and clinical presentation is highly variable, largely dependent on the location of the ABC. In the present case, the patient presented with proptosis and periorbital cellulitis likely due to the expansile nature of the lesion against the lamina papyracea. In the review by Hnenny et al. [5], they report that lesions affecting the skull base are more likely to present with neurological deficits including anosmia, ataxia, otalgia, facial numbness and hearing loss.
Imaging modalities such as CT and MRI are essential to aid both diagnosis and for surgical planning. CT features demonstrate the presence of an expansile, lucent bone lesion with osseous remodelling and cortical thinning [6]. Fluid levels are common and are more readily observed on MRI than CT [7]. The signal characteristics are also dependent on the age of any blood products within the lesion. Other MRI features include the presence of multiple internal septations and a ‘soap bubble’ appearance due to the presence of small cysts projected from larger cysts as in our case. Ultimately, histological evaluation is key and ABCs typically demonstrates irregular, blood-filled chambers with islands of bone and fibrous tissue [8].
Surgical resection is the treatment of choice though complete clearance is sometimes impossible at the skull base. In such cases, further surgical procedures to debulk the lesion may be needed. For refractory cases in adults, limited success with radiotherapy has been reported in cranial ABCs, albeit with an accepted risk of sarcomatous degeneration [4]. However, as there is a paucity of information for ethmoidal lesions particularly in children, there exists no clear consensus for radiotherapy.
CONCLUSION
ABCs are challenging lesions to manage in the head and neck region. Whilst they may not be truly malignant, the proximity of complex anatomical structures means that potential disability from untreated or inadequately treated lesions can be devastating. We propose that ABCs arising within the paranasal sinuses ought to be managed in a highly specialized unit, jointly with both ENT and craniofacial surgery input.
CONFLICT OF INTEREST STATEMENT
None.
LEARNING POINTS
What is already known:
Aneurysmal bone cysts (ABCs) are well known entities in long bones, the pelvis and the spine but are extremely rare in the head and neck region.
Surgical management can be curative but there is a high recurrence rate.
What the article adds:
Diagnosis may be delayed due to the uncommon location of the lesion.
Patients ought to be managed in a multidisciplinary fashion with craniofacial surgery input for optimum surgical management.
Treatment of an ABC in the paranasal sinuses is challenging due to the paucity of literature on consensus management as well as its proximity to crucial anatomical structures.
FUNDING
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.



