-
PDF
- Split View
-
Views
-
Cite
Cite
Ian H Rutkofsky, Raguraj Chandradevan, John T Williams IV, Catherine Collins, Felisha L Kitchen, Craig C Odum, James D Colquitt, Joseph Bear, Patrick Narh-Martey, Cured by Da Vinci Xi: meticulous dissection of an infected urachal cyst presenting with lower urinary tract symptoms in an adult, Journal of Surgical Case Reports, Volume 2018, Issue 12, December 2018, rjy327, https://doi.org/10.1093/jscr/rjy327
Close - Share Icon Share
Abstract
An unusual finding in an adult patient with an infected urachal cyst, was treated surgically using the Da Vinci robot. A 26-year-old woman was admitted to our hospital with complaints of lower abdominal pain and burning sensation with urination. She was diagnosed with lower urinary tract infection, treatment did not help her symptoms and further evaluation of CT revealed complex enhancing mass superior to the urinary bladder. The differentials included inflammatory cause such as an abscess, neoplastic mass, urachal cyst, vitello intestinal fistula and urachal sinus. Da Vinchi robotic diagnostic laparoscopy was performed to obtain an accurate assessment and treatment. After cystoscopy followed by laparoscopic exploration of the abdominal and pelvic cavity further helped to narrow down a diagnosis of remnants of urachus. Pathology of the excised specimen showed inflammation without evidence of malignancy and confirmed Urachal cyst. The patient had an uneventful post-operative course.
INTRODUCTION
Urachal cysts are very rare in adult patients because the urachus is normally obliterated in infancy [1]. After the urachus obliterates it presents as the median umbilical ligament [2]. Normally, this structure presents as a fibrous cord, however, urachal abnormalities such as a vesicourachal diverticulum (3%), umbilical urachal sinus (18%), urachal cyst (31%) and a patent urachus (48%), may occur depending on the location of the originally tubular urachus [3]. A urachal cyst occurs in 0.02% of total live births, but is only clinically relevant in 0.00067% of the population [4].
CASE REPORT
A 26-year-old woman presented to the Emergency Department at our medical center with the complaint of burning while urination, frequency and supra pubic abdominal pain. The symptoms lasted for 2 days. She also complains of nocturia and the pain was constant. The pain did not radiate, 5/10 in the pain scale, and a constant type of pain. She did not have fever, nausea, vomiting or any change in her bowel movements. Her LMP was a week ago and did not have any abnormal vaginal discharge. Physical examination revealed lower abdominal tenderness and tenderness was noted in para-umbilical area. There was not any costovertebral tenderness. During the initial presentation she has underwent several tests including beta hcg, CBC, BMP and UFR. Lap results was abnormal for urinalysis, WBC 10–25, moderate bacteria, moderate mucus, yeast moderate and cervical NAAT was negative for GC and Chlamydia. The Nitrates test was positive and patient had no systemic symptoms and lower urinary tract infection was diagnosed. She had been treated for urinary tract infection over 10 days with antibiotics in the outpatient settings. During the course, she did not feel a complete resolution of symptoms rather she had aggravated symptoms of dysuria, frequency and burning. She denied nausea, vomiting, weight change, palpitations, heat or cold intolerance and peripheral edema. Systematic review of symptoms revealed that she had chronic constipation with hard non bloody stools, around two bowel movements per week and occasionally she uses stool softeners and that helps her to have bowel movements. She denied any history of abdominal trauma and family record of any similar illness related to gastrointestinal tract. Persistence of her symptoms further warranted investigations and she had underwent a CT scan while receiving antibiotic therapy.
Contrast-enhanced computed tomography CT of the abdomen/pelvis with contrast revealed (Fig. 1) demonstrates 4 × 3.3 × 6.8 cm3 multiloculated enhancing hypodense and isodense mass noted extending superiorly from urinary bladder dome with surrounding acute inflammatory stranding and minimal fluid with possible invasion into the urinary bladder dome (Fig. 2). Secondary thickening of adjacent distal small bowel loop also presented with high probability, and thick walled, dense collapsed urinary bladder seen with per vesical stranding. These findings with the clinical presentation was further evaluated and differential diagnosis of patent urachus, urachal sinus, urachal diverticulum and malignant transformation of the cyst was aided and diagnostic laparoscopy surgery was planned.


Coronal plan of CT abdomen/pelvis showing the urachal cyst above bladder.
SURGICAL TECHNIQUE
Patient was administered general anesthesia with placement of endotracheal tube. She was placed in lithotomy position (stirrups), both arms tucked at sides, strap secure across chest and a bair hugger (warmer) was placed around upper chest/head/neck area. Our patient was prepped with betadine for a vaginal/perineal prep and chloroprep was used on the abdomen. After sterile draping of the patient, and official time-out with all in agreeance, the Urologist evaluated the bladder with a cystoscopy using a 70° scope to survey for any persistent urachal abnormalities, and confirmed that no fistula/congenital abnormalities from inside bladder. General Surgeon scrubbed in and proceeded with insertion of veress needle and insufflated the abdominal cavity with CO2. Once the abdominal pressure reached 15 mmHg, General Surgeon used a 5 mm/0° laparoscope inside a 5 mm first-entry trocar and watched himself insert the trocar through each layer until passing through the peritoneum and into the abdominal cavity. Two 8 mm robotic Xi trocars were inserted, a 12 mm AirSeal Assistant port, and the 5 mm first entry port was replaced with a third robotic 8 mm cannula. Altogether 3–8 mm robotic ports, a 12 mm assistant port, and a 30° robotic scope was utilized during the case. Docking of the robot followed port placement with ‘renal right’ selected on the patient cart while the patient was placed in slight Trendelenburg. Da Vinci Xi instruments used were a fenestrated bipolar and a monopolar scissor to begin dissection. Initial survey of abdomen confirmed that there is an extension of a structure from the dome of the bladder to the posterior surface of the umbilicus (Fig. 4) and more suggestive of an infected urachal cyst. Further evaluations revealed that the cyst surrounding the umbilicus is inflamed and had multiple pus filled cavities. A complete resection of the cyst and the connecting structure was resected by Da Vinci Xi robotic system (Fig. 5). The bladder was filled with 300 ml of sterile normal saline mixed with methylene blue dye through the Foley catheter to determine any bladder otomies from the dissection. None were present. Urologist over sewed a thin area of the bladder with a 3-0 vicryl SH suture (Fig. 6). Complete resection of the cyst was performed successfully (Fig. 8). Slight irrigation was used to check for bleeding and the specimen was put in an endocatch bag to be retrieved when ports are ready for removal. A 19 Fr Blake drain was placed in the abdominal cavity and secured with a 2-0 nylon suture. Foley catheter is also indwelling.

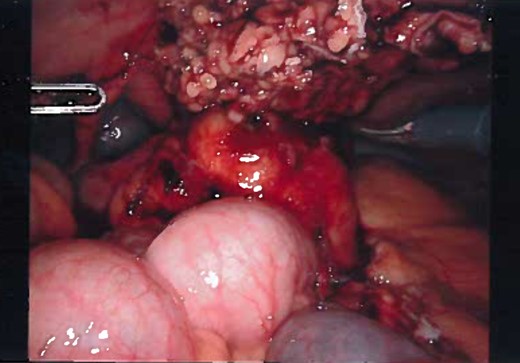
Inflamed and necrotic appearance of the urachal cyst with multiple pus filled cavities.

Laparoscopic view of the urachal cyst, viewing the umbilical portion of the urachus.
Laparoscopic view of the urachus while dissection, view of the dome of the bladder and dissection of median umbilical ligament.
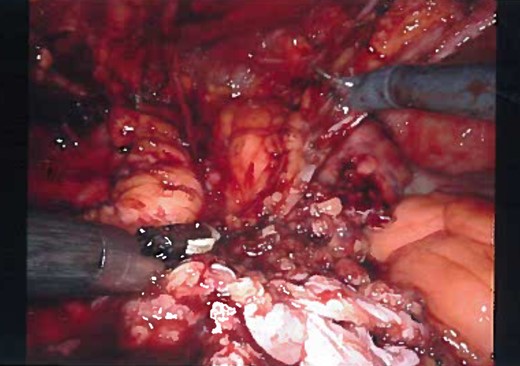
Laparoscopic view of the dissection, most of the cyst is dissected and over-sewing the dome of the bladder.
Gross appearance of the urachal cyst resembled an inflammatory and necrotic appearance with multiple cystic cavities (Figs 3 and 7). On pathology, tentative diagnosis of the specimen was confirmed as an urachal cyst. The appearance of an ulcerated cyst wall noted with marked fibrosis, acute and chronic inflammation with focal abscess, foreign body giant cells, and fibrous adhesions, consistent with history of infected urachal cyst and no evidence of malignancy. Intra-operative culture of urachal cyst provided contents positive for Escherichia coli, and negative for fungal material. The patient had an uneventful post-operative course. We followed up the patient in 2 weeks and again in 3 months in the outpatient clinic. During the follow-up, patient reported that removal of the cyst helped her abdominal pain, urinary tract symptoms have completely resolved and constipation was improve pertinently.

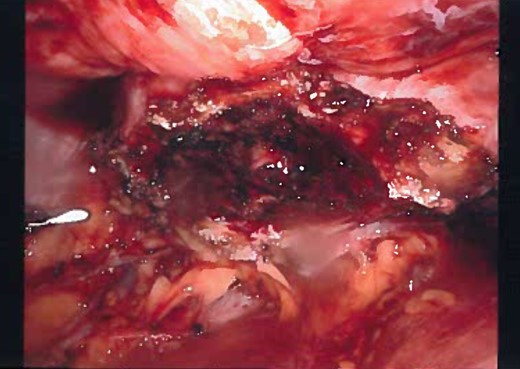
Laparoscopic view of the complete dissection of the cyst before removing the port.
DISCUSSION
The urachus is an embryologic structure that transforms during development and is the upper part of the bladder, both of which arise from the ventral part of the cloaca and allantois [5]. Incomplete regression of the urachal lumen results in several anomalies, and presents as urachal sinus, patent urachus, urachal diverticulum or urachal cyst. An infected urachal cyst is one of pathologies of the urachus, however, all which are rare findings if present in adulthood [6]. Often the presentation is consistent with lower abdominal pain, urinary tract symptoms and with vague symptoms [2]. Ultrasound (US), computed tomography (CT) and magnetic resonance imaging (MRI) are imagining studies that can effectively help identify the urachal pathology [6]. Definitive diagnosis is often made following exploratory laparotomy for an unexplained acute abdomen. Delay in treatment of an infected urachus can lead to complications of infection including sepsis, fistula formation, sinus tract formation or even rupture leading to peritonitis [6]. Treatment is by complete excision, however, the techniques have been debated [6], however, open surgical excision has been the treatment of choice for many years.
Treatment may be a two-stage procedure, involving primary incision and drainage, later followed by urachal remnant and bladder cuff excision or a single-stage operation, which can be performed either open excision or laparoscopically [4, 7]. Remnants found in neonates younger than 6 months of age usually do not require surgical correction as they usually resolve spontaneously [8].
Recently, robotic resection has replaced laparoscopic and open resections because of its high success rate. In addition, robotic procedures can reduce surgical time, exposure to anesthetic agents, lower the rate of post-operative complications and reduce recovery time post-operatively. In cases of an infected urachal cyst presenting with non-specific symptoms as in our presentation, the Da Vinci robotic surgeries gave a three dimensional view of the anatomical abnormality, with minimal invasiveness, free moving arms and trocars for dissection and minimal bleeding, which also allowed for the patient’s rapid recovery. Over 50% of adults with urachal anomalies may have malignant change, requiring extensive surgical intervention with partial or radical cystectomy [9]. Complete excisions is important and should always be considered in adults who are good surgical candidates because malignant transformation of the remnant is possible [10].
CONCLUSION
Although urachal cysts are rare and their preoperative diagnosis is difficult because of non-specific signs and symptoms, the pathology must be considered in the differential diagnosis when mass lesion is seen on the dome of the bladder on imaging and the patient has non-specific abdominal and urinary tract symptoms. They can be successfully managed by complete resection; laparoscopic and by robotic excision. We believe that robotic resection is the preferred treatment for symptomatic Urachal cysts in adults, as the procedure is minimally invasive and provides optimal recovery time. In addition, resection of symptomatic urachal anomalies found adults might lower the risk of malignant transformation. However, malignant transformation rate may be overestimated because those who seek medical care are likely to be symptomatic, while benign, asymptotic cases may have gone unrecognized. Surgical alternatives to midline or para median incision such as laparoscopic and further advanced with robotic urachal cyst excision warrant further data to determine if morbidity is significantly reduced. In this presentation we have shown that Da Vinci Xi robotic urachal cyst excision is a safe alternative to open surgical procedure.
CONFLICT OF INTEREST STATEMENT
None declared.



