-
PDF
- Split View
-
Views
-
Cite
Cite
Sharnice A Koek, Jack Hammond, Gastric outlet obstruction secondary to orbera intragastric balloon, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy284, https://doi.org/10.1093/jscr/rjy284
Close - Share Icon Share
Abstract
Intragastric balloons are used as a temporary restrictive method in obesity to induce weight loss. They are typically recommended when patients have mild obesity and have failed traditional first line treatments of diet, exercise and behaviour modification. We report a case of a 45-year-old female who presented with nausea, vomiting and abdominal pain two weeks following an uncomplicated insertion of an intragastric balloon. Following investigation, she was found to have a gastric outlet obstruction which required endoscopic removal of the balloon. While a rare occurrence, gastric outlet obstruction as seen in this case, highlights the importance of early recognition in order to proceed with swift diagnosis and intervention in order to prevent significant morbidity such as ischaemia and perforation.
INTRODUCTION
In contrast to bariatric surgery, which has significant cost, invasiveness and potentially lifelong side effects, intragastric balloon therapy is a minimally invasive, temporary method of inducing weight loss. It involves endoscopic placement of a soft, fluid filled balloon into the stomach to promote the feeling of satiety and restriction. The intragastric balloon is then endoscopically removed after several months. While minimally invasive, they can lead to significant complications including, rupture and migration of the balloon, bleeding ulcers, gastric outlet obstruction and gastric perforation. We present a case of gastric outlet obstruction secondary to an intragastric balloon.
CASE REPORT
A female patient aged 45 years presented with 2 weeks of right upper quadrant pain. The pain was constant in nature and associated with nausea and non-bilious, non-bloody emesis of undigested food. On review of systems, the patient denied any urinary symptoms, chest pain, dyspnoea or fevers.
She had a significant history of an uncomplicated placement of an ORBERA® intragastric balloon [Apollo Endosurgery, formerly Bioenterics Intragastric Balloon (BIB)] 2 and a half weeks prior to presentation. At the time of the procedure 600 ml of blue saline was placed within the balloon. She otherwise did not have any relevant past medical history and was not on any regular medications. She was a non-smoker and did not drink any alcohol.
Clinically she was apyrexial and haemodynamically stable with a heart rate of 88 beats/min and a blood pressure of 109/70 mmHg. She did not appear to be in any distress and her pulmonary, cardiac and neurological examinations were within normal limits. Her abdomen was soft, distended, and a smooth palpable mass was felt in the right lumbar region. This was tender on palpation. In addition, she was also tender in the right upper quadrant, without any rebound or guarding, and bowel sounds were present.
Laboratory studies including a complete blood count, metabolic panel and lipase were all within normal limits with the exception of a minimally raised C-reactive protein of 10.5 mg/L.
In initial erect chest X-ray was unremarkable for any evidence of pneumoperitoneum. A subsequent contrast abdominal computed tomography (CT) study demonstrated a large intragastric balloon within the gastric antrum, containing fluid and a small amount of gas, measuring 115 mm × 96 mm × 116 mm diameter (Fig. 1). Above this, the gastric fundus and body were moderately distended and contained a fairly large amount of ingested fluid and gas (Fig. 1).
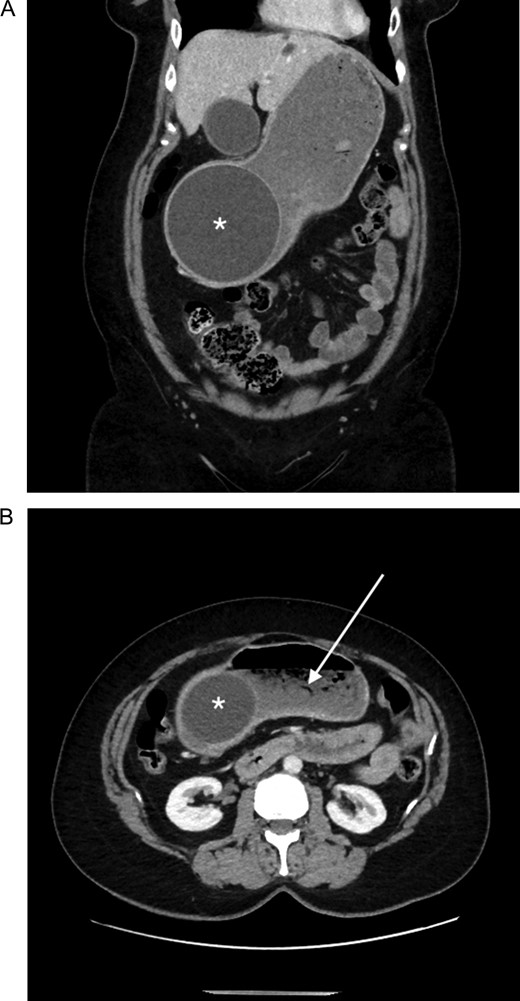
Abdominal computed tomography showing (A) an intragastric balloon within the gastric antrum (asterisk), with (B) a moderately distended fluid and gas filled gastric fundus and body (arrow).
Overnight, she was managed with a nasogastric tube on straight drainage, analgesia and intravenous fluids. The following morning, she successfully underwent an endoscopic removal of the intragastric balloon. During endoscopy, there were no erosions to the oesophagus or ulcers noted within the stomach. Following the procedure, she was commenced on a clear fluid diet for 48 h followed by a soft diet and was discharged the same day with complete resolution of presenting symptoms and gastric outlet obstruction.
DISCUSSION
Due to the significant cost, adverse events, invasiveness and potentially lifelong side effects of bariatric surgery, intragastric balloon therapy offers a minimally invasive, temporary method of inducing weight loss. It is particularly targeted to mildly obese patients with a body mass index of between 30 and 40 kg/m2 who have had unsuccessful attempts of weight management with first line strategies such as diet, exercise and behaviour modification [1]. One of the major benefits of balloon therapy is for patients who may not qualify for bariatric surgery to have early intervention in order to prevent or treat obesity-related medical illnesses [2]. A recent meta-analysis by Imaz et al. [3] of 15 studies, found a 12.2% initial weight loss at the time of balloon removal (6 months) and a decrease in BMI of 5.7 kg/m2.
Intragastric balloons have evolved from their initial introduction in 1985 with the Garren-Edwards Gastric Bubble (GEB; American Edwards Company) [4]. Modern intragastric balloons such as ORBERA®, have a spherical shape, high volume capacity (500–700 ml) and use saline for filling. These have subsequently been associated with a reduced complication rate [5].
Nevertheless, the use of intragastric balloons have been associated with a complication rate up to 5.5% [3]. Approximately 7–9% of patients require early removal due to intolerance [6–8]. Common adverse events include, abdominal discomfort, gastroesophageal reflux, nausea and vomiting [5]. Significant complications may include spontaneous deflation and migration of the balloon, peptic ulcers, gastric outlet obstruction and gastric perforation. Genco et al. [6], report that 0.76% of balloons are complicated by gastric obstruction within the first 2 weeks of placement. This was similar to a finding by Imaz et al. of 0.8% [3]. Most importantly, gastric outlet obstruction secondary to an intragastric balloon may progress to necrosis and perforation emphasizing the need for early recognition and swift intervention [5].
Bariatric therapies are now performed at an increasing rate as a response to the rise in obesity in western populations. While gastric outlet obstruction is a rare occurrence, it is important for both emergency and surgical physicians to be aware of the common presentations of these patients. As noted earlier, vomiting and abdominal discomfort are common symptoms following placement of the balloon, however, a palpable mass in the pylorus and non-bilious vomiting of undigested food may suggest gastric outlet obstruction. Failure to have a high index of suspicion may delay appropriate imaging and diagnosis and lead to increased morbidity. Symptoms should be further investigated with appropriate laboratory tests as well as an abdominal CT to identify appearances of a gastric outlet obstruction and any evidence of subsequent necrosis.
As was undertaken in this case, the initial treatment of choice for intragastric balloon gastric outlet obstruction is for initial resuscitation followed by endoscopic deflation and removal of the balloon. This case report serves to bring awareness of a potential rare complication following intragastric balloon insertion. While patients who present with abdominal discomfort, nausea and vomiting following an intragastric balloon insertion may be easily misdiagnosed as expected post procedure symptoms, it is important to investigate with appropriate laboratory tests and radiological imaging to ensure any complication is identified early to prevent significant morbidity.
ACKNOWLEDGEMENTS
Nil.
CONFLICT OF INTEREST STATEMENT
None declared.



