-
PDF
- Split View
-
Views
-
Cite
Cite
Kshitij Desai, Jason Cook, Evan Brownie, Mohamed Zayed, Tulip piercing the aorta: a rare case of IVC filter aortic perforation and obstruction, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy280, https://doi.org/10.1093/jscr/rjy280
Close - Share Icon Share
ABSTRACT
Prolonged implantation of inferior vena cava (IVC) filters can lead to significant morbidity. We present a 25-year-old man with antiphospholipid syndrome, lower extremity deep vein thrombosis, and subsequent Gunther-Tulip IVC filter placement. More than 10 years following IVC filter placement he developed progressive abdominal and back pains. Cross-sectional angiography revealed that he had a chronic IVC occlusion, and IVC filter limb extensions into the infrarenal aorta, lumbar spine, and right psoas muscle. The IVC filter limb protruding into the aorta had also pierced through the backwall to lead to partial lumen thrombosis and obstruction. The patient underwent a transabdominal exposure of the infrarenal IVC and aorta, filter explantation and aortic patch angioplasty repair. This case highlights the severity of aortic injury from a protruding IVC filter limb that necessitated open aortic repair. Improved selection, monitoring and retrieval stewardship of IVC filters can help reduce the risk of unintended aortic complications.
INTRODUCTION
The rate of retrievable inferior vena cava (IVC) filter implantation has significantly increased over the past decade [1]. In 2015, it was estimated that >44 000 filters were implanted [1]. The 2016 American College of Chest Physician (ACCP) guidelines supported the use of IVC filters in patients who suffer from acute venous thromboembolic event (VTE) and have failed or cannot tolerate anticoagulation therapy [2]. However, current guidelines are unclear about when to choose a permanent versus retrievable IVC filter, the duration of filter implantation, and protocols for surveillance once a retrieval filter has been placed. A recent FDA advisory was issued warning against inadequate retrievable IVC filter surveillance post-implantation [3]. Accordingly, recent reports have cited potential aortic complications that may result from prolonged retrievable IVC filter implantation [4, 5]. Here we present a unique case of prolonged IVC filter implantation for over 10 years leading to aortic perforation and partial thrombosis.
CASE REPORT
A 25-year-old man presented to attention with progressive intermittent abdominal and back pains. The patient had a history of antiphospholipid syndrome, who 10 years ago developed a recurrent pulmonary embolus (PE) and lower extremity deep venous thrombosis (DVT) despite therapeutic anticoagulation. He was treated with daily Rivaroxaban therapy and a retrievable Gunther Tulip (Cook, Inc., Indianapolis, IN) IVC filter was placed in his infrarenal IVC. At the time of presentation, the patient had an unremarkable exam, but a CTA demonstrated a segmentally occluded distal infrarenal IVC (Fig. 1A). The IVC filter limbs were protruding out of the small atretic IVC, and extending into the infrarenal aorta, L3 vertebral body and right psoas muscle (Fig. 1). The IVC filter limb protruding into the aorta was also piercing the aortic backwall, and was a nidus for partial thrombosis and stenosis of the aortic lumen (Fig. 1B and C). Given the patient’s symptoms and severity of filter limb injury into the aorta, the patient was offered an open explantation of the IVC filter and repair of the infrarenal aorta (Fig. 2).
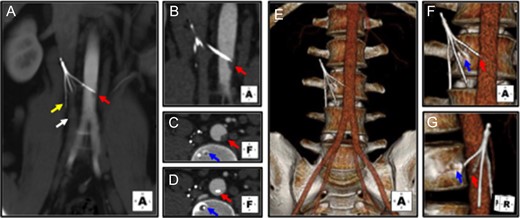
Preoperative CTA demonstrates Gunther Tulip IVC filter perforation of the infrarenal aorta, lumbar spine and psoas muscle. (A) IVC filter in occluded atretic appearing infrarenal IVC (white arrow). IVC filter legs are protruding out of the IVC wall, embedding into the adjacent right psoas muscle (yellow arrow), and adjacent infrarenal aorta (red arrow). (B) Coronal view demonstrates partial obstruction of the aortic lumen at the tip of the perforating IVC filter leg (red arrow). (C and D) Transverse cross-sectional views demonstrates protrusion of filter leg in aorta and partial obstruction of aortic lumen (red arrows), as well as embedding of one of the filter legs into the L3 vertebral body (blue arrows). (E–G) Three dimensional reconstructions also demonstrate protrusion of the IVC filter legs into the aorta (red arrows), and lumbar spine (blue arrows).
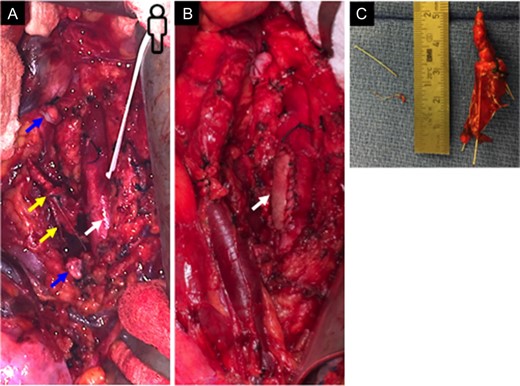
Open operative IVC filter explantation and aortic repair. (A) Transabdominal exposure of the infrarenal aorta (white arrow). The chronically occluded infrarenal IVC was segmentally ligated and transected (ligated ends indicated by blue arrows). Tilted IVC filter is visualized adjacent and attached to the infrarenal aorta (yellow arrows). (B) Successful explantation of IVC filter and repair of infrarenal aorta with a bovine pericardial patch. (C) Explanted IVC filter body with associated dense fibrous tissue, as well as leg fragments removed from the infrarenal aortic lumen.
Operative repair was performed through a ventral mid-line laparotomy incision, left lateral mobilization of the right colon by dividing the white line of Toldt, and Kocher maneuver mobilization of the duodenum. The underlying infrarenal vena cava and aorta were each visualized and exposed along their lengths to facilitate proximal and distal control of the area involving the IVC filter. The atretic chronically occluded distal IVC was proximally and distally ligated and transected. The IVC filter was mobilized with care and a wire cutter was used to dissociate it from the limbs embedded in the aorta and lumbar spine. The filter limb embedded in the lumbar spine was highly fibrosed and was left in place in the bone. The infrarenal aorta was proximally and distally clamped and a ventral arteriotomy was made to facilitate removal of remaining filter leg. Dorsal aortic luminal thromboendarterectomy and ventral wall patch angioplasty with bovine pericardium was performed. The patient recovery was unremarkable, and he was maintained on therapeutic anticoagulation. Postoperatively, a CTA at 3 months demonstrated a stable repair and patent infrarenal aorta (Fig. 3).
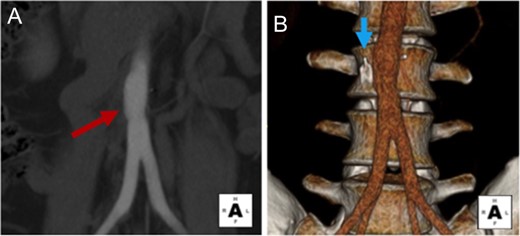
Postoperative CTA demonstrates stable aortic repair. (A) Coronal views demonstrate patent infrarenal aorta and patch angioplasty repair site. (B) 3D reconstruction demonstrates normal caliber infrarenal aorta, and residual IVC filter leg embedded in the L3 vertebral body.
DISCUSSION
Retrievable IVC filter complications include migration, thrombosis, filter fracture and perforation of adjacent structures. It is estimated that 40% of filter limbs that erode through the IVC wall can lead to perforation of the duodenum, spine and aorta. However, a recent review suggested that prolonged placement of IVC filters designed with or without implantation limbs can lead to aortic pathology [6].
We present here a very unique case with an IVC filter dwell time of over 10 years. This is the longest reported in recent literature. Other cases reporting aortic injury from IVC filters have documented implantation periods of 2 to 9 years [5–7]. We predict that in this patient’s case the long filter dwell time caused slow IVC scarring, thrombosis, atresia and eventual perforation of the filter limbs through the residual IVC wall. As discussed in prior reports [5], this likely led to the protrusion of the filter limbs into adjacent structures such as the spine, psoas muscle and aorta. We suspect that luminal trauma along the aortic backwall led to scarring that served as a nidus for partial luminal thrombosis and obstruction.
This case highlights the severity of potential aortic injury with both perforation and partial aortic lumen thrombosis. Aortic injury resulting from IVC filter preformation often necessitates an operative repair [4, 7]. In this case we observed that a transabdominal mid-line approach for a left lateral mobilization of the right colon, and Kocher maneuver mobilization of the duodenum, provided maximal exposure of both the infrarenal aorta and IVC. Filter extraction from the aorta necessitated standard aortic clamping maneuvers, open exploration of the aortic lumen and patch angioplasty repair. Recovery from this operation is well tolerated, and resumption of postoperative chronic anticoagulation therapy was feasible.
The frequency of IVC filter complications may increase over the next decade given the low reported retrieval rates of IVC filters [8, 9]. IVC filter retrieval protocols and decision algorithms are recommended to aid in future patient surveillance, monitoring and filter retrieval [3, 9]. Better stewardship of IVC filter implantation, clinical follow-up, and retrieval may help reduce rates of long-term IVC filter complications [6]. Moreover, the FDA-endorsed, prospective, multi-center, PRESERVE Trial will be the first to evaluate the safety and effectiveness of current commercially available retrievable and permanent IVC filters in subjects with the clinical need for mechanical prophylaxis for PE [10]. It is anticipated that this trial will help determine how well filters prevent PEs and when retrievable filters should be removed—thus, advancing patient safety and help avoid severe complications such as the one described in this report.
CONFLICT OF INTEREST STATEMENT
All authors of this article declare no conflicts in any regard. All authors of this article did not receive any financial support or award for this report.
ACKNOWLEDGEMENTS
We thank Mrs Ronnie Eugea and Mrs Theresa Belgeri for assistance with this case report.



