-
PDF
- Split View
-
Views
-
Cite
Cite
Roy Hajjar, Audrey Létourneau, Margaret Henri, Françoise Heyen, Jean-François Latulippe, Madeleine Poirier, Jean-François Tremblay, Jean-Sébastien Trépanier, Yves Bendavid, Cholecystocolonic fistula with a giant colonic gallstone: the mainstay of treatment in an acute setting, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy278, https://doi.org/10.1093/jscr/rjy278
Close - Share Icon Share
Abstract
A cholecystoenteric fistula (CEF) is a rare complication of cholelithiasis with cholecystitis. Cholecystocolonic fistulas (CCFs) account for 8–26.5% of all CEFs. CCFs can cause colonic bleeding, obstruction or perforation, with such complications being mainly reported in the narrower sigmoid colon. Colonic biliary ileus, or obstruction due to the colonic gallstone impaction, is extremely rare in the proximal colon and its best management is yet to be elucidated. We present the case of a 73-year-old male patient with multiple comorbidities and previous abdominal surgeries who presented with hematochezia and intestinal obstructive symptoms. Imaging revealed a giant 5 × 7 cm2 gallstone in the proximal transverse colon. Laparotomy and stone extraction via colotomy were performed. Complicated proximal colonic gallstones are exceedingly rare with several operative and non-operative treatments already described. A time-saving surgery in a patient with serious comorbidities is reasonable when compared to a more extensive procedure including enterolithotomy, cholecystecomy and fistula closure.
INTRODUCTION
A cholecystoenteric fistula (CEF) is a rare complication of cholelithiasis with associated cholecystitis. Its incidence ranges from 0.5 to 0.9% in surgeries for non-malignant biliary disease [1–3]. It is defined as a connection between the gallbladder and the gastrointestinal tract. Cholecystoduodenal fistulas account for ~75% of all CEFs, followed less commonly by cholecystocolonic and cholecystogastric fistulas [1, 3].
Cholecystocolonic fistulas (CCFs) account for 8–26.5% of all CEFs [1, 2, 4]. They have a female predominance and are incidentally found in 0.06–0.014% of cholecystectomy procedures [4].
CCFs can occasionally cause colonic bleeding, obstruction or perforation. Colonic biliary ileus, or obstruction due to the colonic gallstone impaction, is rare and occurs mainly in the narrower sigmoid colon [4]. Various surgical treatments of complicated and uncomplicated CCF have been described, but its optimal management remains uncertain.
CASE PRESENTATION
A 73-year-old male patient presented to the emergency room (ER) with vomiting, abdominal pain and bloody diarrhea. His past medical history includes arterial hypertension, coronary artery disease, peripheral vascular disease, polycystic kidney disease, end-stage renal disease and superior vena cava thrombosis on warfarin therapy. His surgical history includes an abdominal aortic aneurysm repair and a right nephrectomy. Seven months prior to the events, the patient was admitted for acute calculous cholecystitis and cholangitis that were managed with sphincterotomy and choledocolithiasis extraction via endoscopic retrograde cholangiopancreatography, followed by percutaneous cholecystostomy. It is worth noting that a large gallstone was present in the gallbladder when the patient has undergone an abdominopelvic CT scan 9 years prior to the current episode for an unrelated condition (Fig. 1).

Giant gallstone located in the gallbladder on abdominopelvic CT scan.
The patient presented to the ER complaining of abdominal pain, vomiting, and one abundant bloody diarrhea. His abdomen was distended with diffuse tenderness on physical examination. His vital signs were unremarkable except for a heart rate at 115/min. An abdominopelvic CT scan was performed, and showed a CCF with the giant 5 × 7 cm2 gallstone in the proximal transverse colon (Fig. 2). Oral contrast did not reveal any cholecystoduodenal communication. Blood tests revealed the following: white blood count 11.8 × 109/L, hemoglobin 145 g/L, creatinine 786 μmol/L, international normalized ratio (INR) 2.71 and normal alanine transaminase, aspartate transaminase, bilirubin, alkaline phosphatase and lipase.
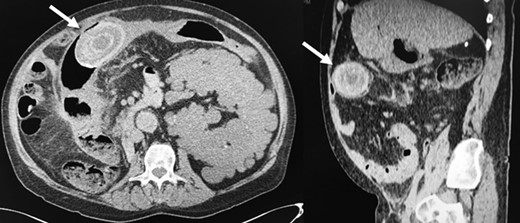
Giant gallstone located in the proximal transverse colon on abdominopelvic CT scan.
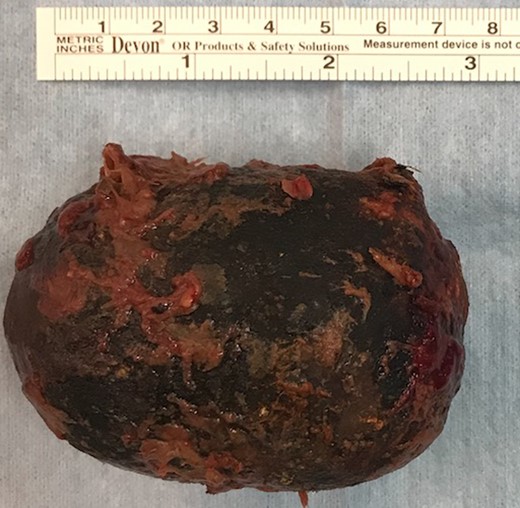
With vomiting and bowel distension suggestive of bowel obstruction, and hematochezia, the patient was taken to the operating room after prompt warfarin reversal with Beriplex®. A supraumbilical median laparotomy was performed and the gallstone identified in the transverse colon. A longitudinal colotomy was performed 15 cm proximal to the impaction site and the gallstone retrieved without any trauma to the surrounding bowel wall (Fig. 3). Local inspection revealed no signs of ischemia or bleeding. The colotomy incision was then closed. The patient was transferred to the intensive care unit for postoperative surveillance. He recovered uneventfully and was discharged after 3 days. The patient was admitted 10 days later for recurrent hematochezia. A colonoscopy was performed and showed a fibrotic and ulcerated cavity in the proximal transverse colon, suggestive of the fistula site, with no other colonic lesions. No active bleeding was present and warfarin was safely resumed.
DISCUSSION
We hereby present a rare case of a giant colonic gallstone lodged in the transverse colon and associated with lower gastrointestinal bleeding and gallstone ileus.
Gallstone ileus accounts for ~1–4% of intestinal obstruction cases, with the occlusion occurring mostly in the terminal ileum or the ileocecal valve [5]. This condition is associated with high morbidity and mortality [6]. Therapeutic surgical strategies include a damage-control enterolithotomy, or a more extensive one-stage procedure, including enterolithotomy, cholecystecomy and fistula closure. Reisner and Cohen [6] reported low morbidity after enterolithotomy alone with a <5% risk of gallstone ileus recurrence and only 10% of patients requiring surgical reintervention for persistent symptoms. This confined intervention, performed usually in fragile elderly patients with multiple comorbidities, has proven to be efficient and safe. Due to the scarcity of this entity, no formal recommendations exist on optimal management in an acute setting.
Colonic biliary ileus is even scarcer, with the majority of cases reporting sigmoid obstruction. Farkas et al. [5] have recently reported a wide array of surgical interventions that have been previously used to manage gallstone sigmoid ileus, including enterolithotomy, caecostomy, Hartmann’s procedure and bowel resection. Non-surgical measures such as endoscopy and lithotripsy have also been described [5, 7]. Their use with a colonic gallstone obstruction has been suggested as a less invasive option in properly selected patients [5, 7]. It has however been reported that the stone size is not correlated to the success of non-operative management [5]. Although the size of the lithiasis has not been reported as a factor in the success of these treatments, one can wonder if these non-surgical modalities are appropriate. Indeed, in cases of giant stones located proximally in the colon, fragmentation and extraction would be challenging, and endoscopic overinflation of the proximal colon may increase risks of perforation in the presence of mechanical obstruction.
On another note, laparoscopy has been described repeatedly as safe and efficient in the management of CEF and CCF, even when gallstone ileus is present [3, 5]. The benefits of this modality should be weighed against its risks especially that patients with complicated CEFs or CCFs may be too fragile to tolerate a pneumoperitoneum. Moreover, laparoscopy makes the search for other stones in the complete digestive tract more challenging. In our case, a laparoscopic approach was not chosen not only because of its systemic effects, but also because of the previous abdominal surgeries and significant bowel dilatation.
Delayed surgeries addressing the fistula are controversial. They are usually associated with significant morbidity and mortality and are thus considered in patients who could safely benefit from them to prevent recurrence [8].
To conclude, complicated colonic gallstones are extremely rare with the majority of documented cases reporting sigmoid obstruction. Although several therapeutic modalities have been described, no clear consensus on the best management exists. A symptomatic giant gallstone in the transverse colon is an exceptional event and a conservative time-saving surgery in a patient with many serious comorbidities is reasonable. Delayed fistula-oriented interventions may be considered where the risk of recurrence outweighs the risk of a surgery.
CONFLICT OF INTEREST STATEMENT
None declared.



