-
PDF
- Split View
-
Views
-
Cite
Cite
Fernando X Moyon, Miguel A Moyon, Jorge F Tufiño, Alberto Yu, Oscar L Mafla, Gabriel A Molina, Massive retroperitoneal dedifferentiated liposarcoma in a young patient, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy272, https://doi.org/10.1093/jscr/rjy272
Close - Share Icon Share
Abstract
Liposarcomas are rare malignant tumors that mostly develop in the retroperitoneum. They have a broad behavioral spectrum, from small masses of tissue to highly aggressive tumors. The dedifferentiation process occurs in up to 10% and it’s most likely to occur in the retroperitoneum, a process that not only changes its components but also its prognosis. These tumors can grow to a massive size since most of them do not give any symptoms until they invade the adjacent structures. Timely detection and surgery could avoid all these potentially lethal scenarios. We present a case of a 34-year-old patient, who reported a growing mass in her abdomen that reached massive proportions but remained untreated due to lack of sufficient access to healthcare facilities in her geographic location. After complete removal of the mass the patient underwent complete recovery, dedifferentiated liposarcoma was the final diagnosis.
INTRODUCTION
Soft tissue sarcomas are an extremely rare malignancy accounting only 1% of all tumors in adult patients [1]. Liposarcomas are the most common type of sarcomas arising in the retroperitoneum that could become life-threatening [2, 3]. These tumors can grow to a massive size and involve adjacent structures that could make their control even more difficult [4]. Surgery is the treatment of choice as full resection with negative margins could be curative [1].
We present a case of a 34-year-old patient, with a considerable mass in her abdomen. However, due to the lack of sufficient access to healthcare, she did not seek any medical attention. After complete removal of the mass the patient underwent complete recovery, dedifferentiated liposarcoma (DDL) was the final diagnosis.
CASE REPORT
Patient is a 34-year-old female without past medical history. Two years before she sought medical attention for the first time, she noticed a mass in her upper abdomen that has grown to gigantic proportions, however, due to a lack of adequate access to healthcare facilities in her geographic location she did not visit a healthcare professional. In the 4 months previous to seeking medical attention, she noticed pain around the mass, severe weight loss and recurrent episodes of postprandial vomit, which prompted her family to take her to the emergency room. On clinical examination, a malnourished and dehydrated patient with a giant mass in the upper abdominal was discovered. She reported a slight pain on palpation, but no tenderness was encountered. Blood work was normal and due to the size of the mass, an abdominal contrast-enhanced computerized tomography (CT) was requested. It revealed a huge 40 × 28 × 10 cm3 encapsulated retroperitoneal tumor with a soft tissue density (19–30 UH), and an area containing a calcification (Fig. 1A). The mass extended from the right flank to the pelvis. It displaced the liver, right kidney and most of the bowel (Fig. 2A). Yet, it did not invade any adjacent structures and no other masses were observed. Due to these findings and after adequate reanimation, surgery was decided. At laparotomy, a 40 × 30 × 10 cm3 reddish soft consistency retroperitoneal mass was encountered (Figs 3A and 1B), the mass was firmly attached to the third portion of the duodenum, right kidney and ureter. Nevertheless, it did not invade any of the latter (Fig. 2B). No other masses or lymph nodes were encountered. From there surgical decision was straightforward, and complete excision of the mass was performed. During the procedure, an adhesion between the mass and the third portion of the duodenum was tractioned, and a small traumatic duodenal injury occurred. However, due to prompt intervention, the lesion was identified and repaired. A drain was left near the duodenal injury and another one in the retroperitoneal space. After this, the remainder of the procedure continued without any complications (Fig. 3B).
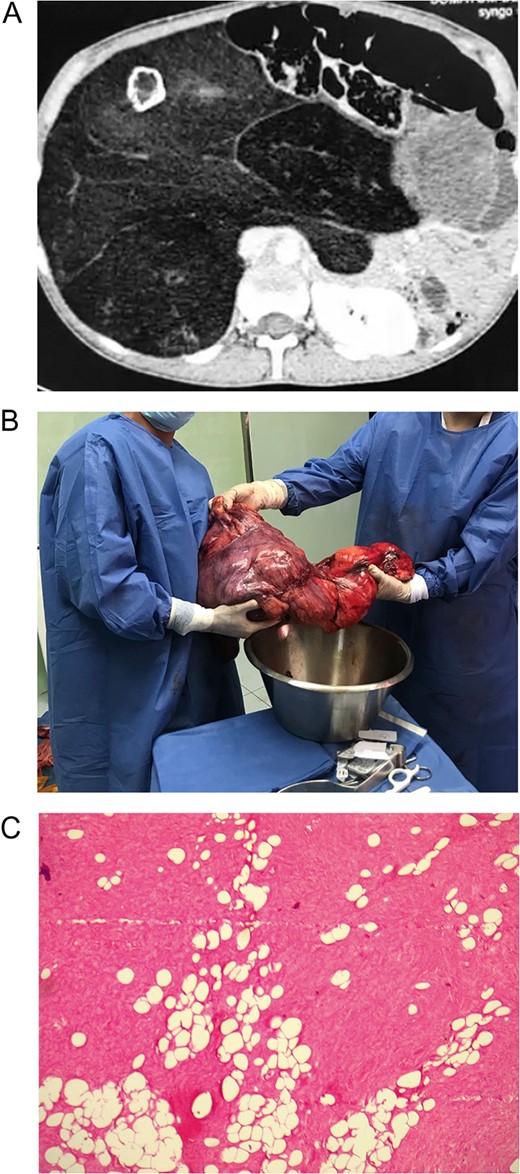
(A) Abdominal CT revealed a huge encapsulated retroperitoneal tumor with a soft tissue density, and an area containing a calcification. (B) Massive retroperitoneal dedifferentiated liposarcoma. (C) Mature adipocytes with some enlarged atypical nuclei.
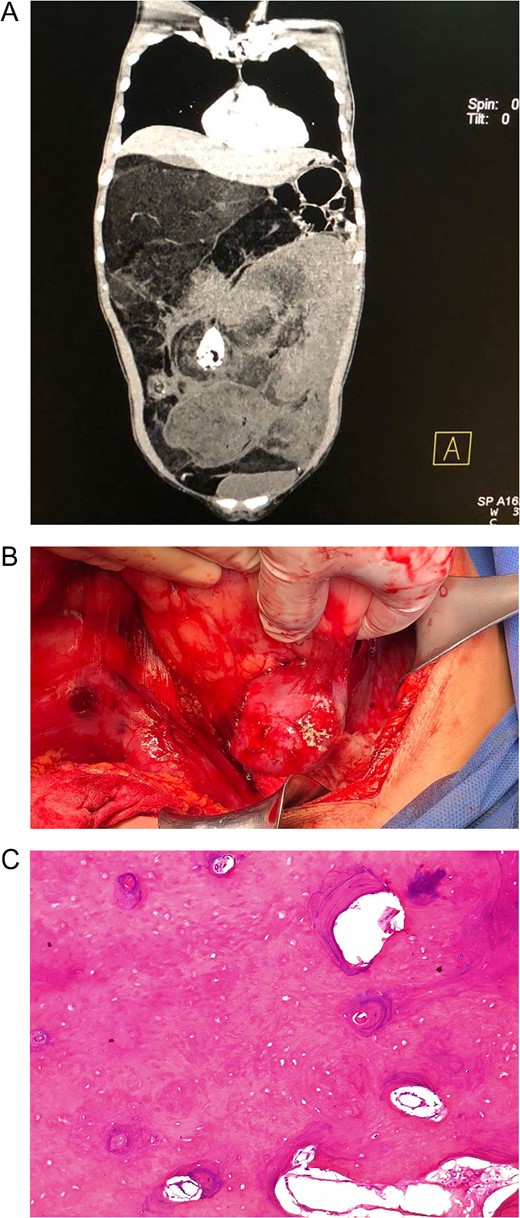
(A) Abdominal CT: Retroperitoneal tumor that displaced the liver, right kidney and most of the bowel. (B) Giant retroperitoneal mass, the mass had multiple adhesion to adjacent organs making dissection troublesome. (C) Transition towards a fusiform cell sarcoma and areas of benign ossification.
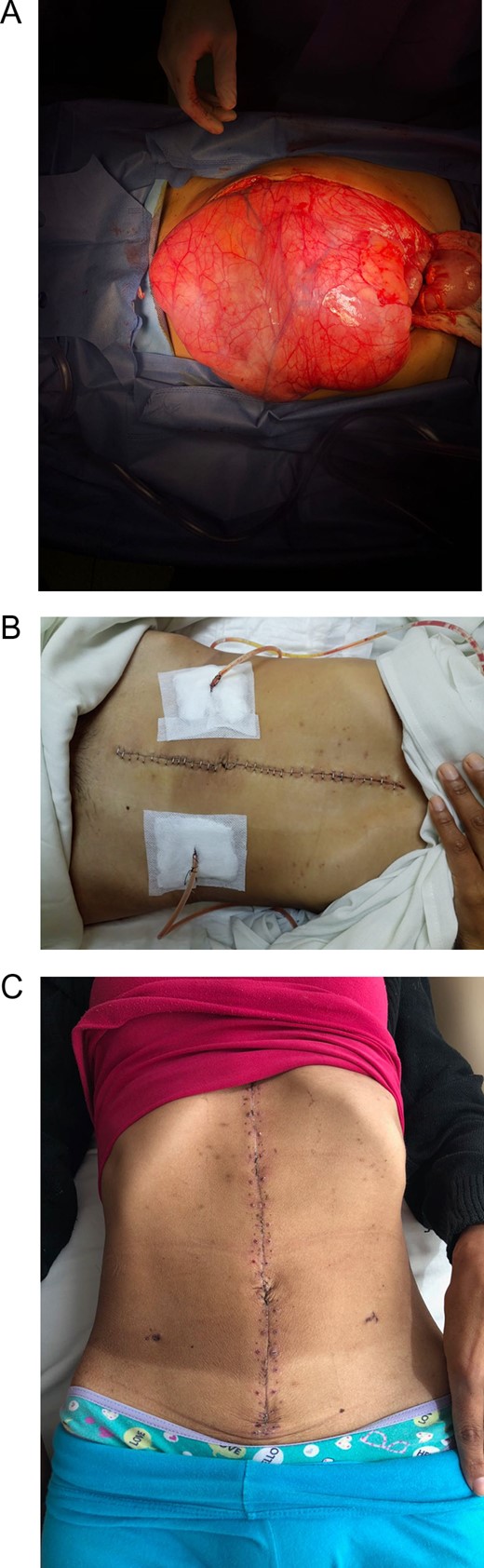
(A) Giant reddish soft consistency retroperitoneal mass. (B) Abdomen, after successful surgery, the mass was resected and the drains were left in place. (C) Patient on follow-up controls.
Pathology reported a DDL, the tumor was composed of mature adipocytes with some enlarged atypical nuclei (Fig. 1C). In some areas, the liposarcoma transitioned towards a fusiform cell sarcoma and in one area it showed a benign ossification (Fig. 2C). The resection margins were free of tumor tissue.
The postoperative period of the patient was uneventful, 7 days after surgery, the nasoenteric tube was withdrawn and sips of liquids were initiated. Attaining good oral tolerance, antibiotics were withdrawn, abdominal drains were removed and a soft diet was initiated.
The patient was discharged in good conditions. On follow-up controls the patient is doing well and is undergoing periodic controls with an oncology specialist (Fig. 3C).
DISCUSSION
Soft tissue sarcomas are an extremely rare malignancy accounting only 1% of all the tumors in the adult population [1]. Liposarcomas are the most common type of sarcomas arising in the retroperitoneum (12–40%), nonetheless they can occur wherever fat is present. They are thought to arise due to genetic abnormalities [1–3] and have a wide behavioral spectrum, from well-differentiated tumors that lack the capacity to metastasize, to tumors with dedifferentiated components which behave in a more aggressive manner. This dedifferentiation process occurs in up to 10% of the cases and it’s most likely to occur in the retroperitoneum [1]. Yet the mechanisms responsible for this progression are not completely understood [4].
Ever since the first description by Evans et al. in 1979, more tumors are now more often classified under the dedifferentiated group [5]. DDLs show a transition from a well-differentiated liposarcoma to a sarcoma of variable histologic grade [3, 6]. However, reactive or metaplastic bone formations should not be confused with a real osteosarcomatous differentiation [5], as it was discovered in our patient.
The extension of the dedifferentiated component and its mitotic index is relevant as it changes the prognosis, metastatic rates and local recurrence [1, 3]. Furthermore, patients who have tumors arising from the retroperitoneum tend to have significantly worse survival rates than those with tumors at other anatomic sites [6, 7]. Retroperitoneal DDLs mostly occur in middle-aged adults with no clear sex or racial correlations [1]. The rate at which these tumors grows varies greatly from case to case, and due to the large potential space in the retroperitoneum, DDLs in this area tend to grow to very large sizes before they produce symptoms [8]. For this reason, most of them present as a painless mass. However, when they produce symptoms they are usually non-specific; abdominal pain, and early satiety being the most common. Local invasion of the retroperitoneal structures can produce neurological, musculoskeletal and obstructive bowel disorders [2, 3]. CT is the gold standard when it comes to diagnosis, staging and preoperative evaluation of DDLs [2].
In our case, the diagnosis was delayed due to her lack of access to healthcare, despite the patient noticing the mass. This delay in the identification, diagnosis and treatment lead to a more complex scenario with a more troublesome yet efficient procedure.
Retroperitoneal liposarcomas are potentially curable with complete resection of the tumor with negative margins [9] nevertheless complete resection of these tumors is often challenging, as these lesions are very large when diagnosed and may involve many adjacent organs and structures due to the tumor size [2, 6]. The prognostic factor most consistently associated with survival and recurrence is the complete surgical resection with negative margins [10]. That being said due to the highly aggressive nature of retroperitoneal DDLs complementary therapy is usually necessary in spite of obtaining clear surgical margins [1, 2].
DDLs are highly heterogeneous neoplasms with an aggressive behavior that can grow to massive proportions if left untreated. Appropriate identification of this pathology along with a precise surgical technique can benefit the patient prognosis, especially for cases that lack access to healthcare. In addition this case report shows that complications arising during this kind of surgery can be managed through correct and rapid identification of the issue at hand, and that accurate treatment can prevent potentially fatal outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.



