-
PDF
- Split View
-
Views
-
Cite
Cite
Johanna C F Willburger, Christoph Kettelhack, Bruno Fuchs, Dirk J Schaefer, Rik Osinga, Giant myxoid liposarcoma of the gluteal region: case report of patient caused delay of surgical treatment and review of the literature, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy265, https://doi.org/10.1093/jscr/rjy265
Close - Share Icon Share
Abstract
Although adult soft tissue sarcoma is a rare disease, it needs individual treatment by an experienced, interdisciplinary team. We present an exceptional case of a 36-year-old woman suffering from a giant intermediate grade myxoid liposarcoma of the left buttock. She had been seen 4 years earlier but refused to undergo any treatment by then. Now suffering from a foul, ulcerating and superinfected tumor she agreed to surgical treatment. Despite delay, treatment could be performed according to the most up to date sarcoma guidelines which are discussed, including a brief review of the literature.
INTRODUCTION
Adult soft tissue sarcomas are rare tumors, with an estimated incidence averaging 4–5/100 000/year in Europe [1]. Adipocytic tumors represent the largest subgroup, of which liposarcoma is the most common [2]. The unusual clinical course over a 4-year time span of a slowly growing, eventually necrotizing, untreated gluteal myxoid liposarcoma in a young Swiss woman is described and the outcome after surgery reported.
CASE REPORT
A woman 36 years of age presented with a painless, slowly growing mass of the left buttock (Fig. 1). Magnetic resonance showed an inhomogeneous tumor of 10 × 8.5 × 6 cm3 in size suspicious for myxoid sarcoma (Fig. 2). Biopsy was recommended. However, the patient refused and was lost for follow-up. Three an a half years later, the anemic patient was referred again, now with a giant 22 × 19 × 24 cm3 measuring, foul, ulcerating and bleeding tumor (Fig. 3), partly infiltrating the gluteus maximus muscle (Fig 4). Myxoid sarcoma was confirmed by three deep punch biopsies in local anesthesia followed by swift surgical resection.

Clinical situation in September 2014. The patient noticed a slowly growing, painless mass on her left buttock.
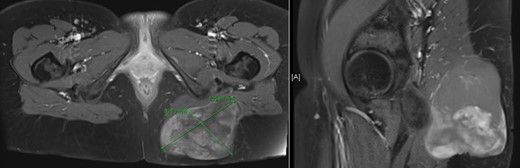
Magnetic resonance imaging described a left gluteal tumor, partly situated within the left gluteus maximus muscle, without infiltrating the skin.

Clinical situation in March 2018 (3 and a half years after primary finding). A gigantic tumor arose of the left gluteal region, partially necrotic, foul and with bleeding ulceration.
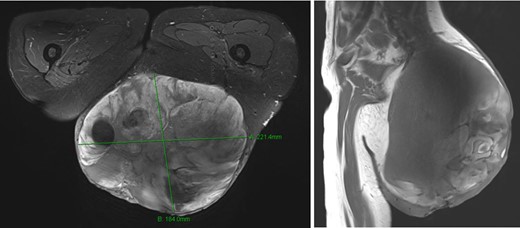
Magnetic resonance imaging showed a very large tumor of the left gluteal region, further infiltrating the left gluteus muscle and now with infiltration of the skin.

The patient was put in prone position under general anesthesia and the operating site desinfected with Povidone Iodine solution. The operation field was additionally covered with an Iodine impregnated incision drape to further minimize bacterial contamination. The skin was incised circumferentially, minimally 1 cm away from the palpable tumor mass, until reaching the fascia of the gluteus maximus muscle. The tumor was then resected circumferentially including parts of the gluteus maximus muscle and its fascia leaving the sciatic nerve and the external anal sphincter untouched. Wound closure was achieved after epifascial mobilization, followed by uneventful wound healing and an acceptable aesthetic result (Fig. 5). Pathohistological workup confirmed wide resection (R0) of an intermediate grade myxoid liposarcoma Grad 2 according to the French Federation of Comprehensive Cancer Centers (FFCCC), weighing 5.6 kg and measuring 26 × 24 × 15 cm3. After interdisciplinary discussion at the in-house sarcoma board, no radiation therapy was recommended.
DISCUSSION
At first encounter with an experienced tumor surgeon, the patient denied to take biopsies due to personal conviction and was lost for follow-up. Four years later, the tumor had grown enormously, was partially necrotic and infected in an anemic patient due to constant bleeding. Nevertheless, the patient could be treated according to the guidelines from the European Sarcoma Network Working Group for soft tissue sarcomas [3].
To recapitulate, these emphasize that surgery is the standard treatment and must be carried out by a surgeon specifically trained in sarcoma treatment.
Standard surgical procedure is wide excision with negative margins (R0), implying the removal of the tumor with a rim of normal tissue around it.
The cut-off for minimal margin on fixed tissue is depending on several factors (histological subtype, preoperative therapies and presence of resistant anatomical barriers such as muscular fasciae, periosteum and epineurium). In the case presented, tumor invasion into the right gluteal muscle indicated extension of the resection margin into that muscle.
Radiotherapy is recommended after wide excision as standard treatment of high-grade, deep and lesions larger than 5 cm. Is the tumor resected and the compartment contained, radiation therapy is not indicated. Despite infiltration of the tumor into the gluteus maximus muscle R0 resection was achieved. After interdisciplinary discussion radiotherapy was not recommended.
Adjuvant radiotherapy is the standard treatment of high-grade (G2–3) sarcomas [4] and mostly recommended in lesions >5 cm, especially when locallized deeply.
Of note, any adjuvant treatment was vehemently refused by the patient.
Formulating any prognosis is challenging, especially since the patient did refuse to undergo any pre- or post-operative staging procedures. The effect of delayed treatment on outcome is discussed controversially [5]. Nonetheless, extended size and depth can influence outcome negatively [6]. However, the intermediate graded tumor of the extremities [6] remained untouched during the entire procedure and was entirely (R0) resected. The patient was treated congruent to the most up-to-date sarcoma guidelines. Therefore we have reason to believe that the patient has a fair chance of being cured.
CONFLICT OF INTEREST STATEMENT
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.



