-
PDF
- Split View
-
Views
-
Cite
Cite
Berta Barbosa, Bruno Santos, Isabel Mesquita, Mário Marcos, Carlos Nogueira, Jorge Santos, Adenocarcinoma arising in a colonic interposition after esophagectomy for benign stricture and review of the literature, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy264, https://doi.org/10.1093/jscr/rjy264
Close - Share Icon Share
Abstract
Colon interposition in oesophageal replacement after oesophagectomy for benign strictures is associated with significant perioperative complications that carry high morbidity and mortality. Long-term sequelae such as further strictures and colonic redundancy are frequent. Adenocarcinoma in the colonic graft is rare. A 70-year-old female presented to our clinic with symptoms of dysphagia. When she was 51 years, she underwent left colonic oesophageal interposition for an oesophageal stricture caused by caustic ingestion. Studies revealed colonic adenocarcinoma in interposed colonic graft, with latero-cervical lymph nodes. She was proposed to neoadjuvant chemotherapy. Although long-term risk analysis is lacking, it’s not unreasonable to propose endoscopic screening according to general colonic cancer guidelines in patients with colonic interposition in oesophageal replacement after oesophagectomy.
INTRODUCTION
Colonic interposition in oesphageal replacement after oesophagectomy is a procedure practiced for the management of both benign and malignant diseases of the oesophagus, particularly when gastric pull-up is not feasible, and its associated with significant perioperative complications that carry hight morbidity and mortality [1, 2].
The environmental changes that occur to an interposed colon, in contrast to its natural milieu, may help promote dysplastic change and augment precancerous conditions [3].
Malignant tumor of the transposed colon is a rare occurrence.
We present a patient who was diagnosed with adenocarcinoma of the colonic graft 19 years after surgery for benign oesophageal stricture.
CASE REPORT
A 70-year-old female presented to our clinic in July 2017 with symptoms of progressive dysphagia for last 3 months.
At the age of 51, the patient was submitted to total oesophagectomy, with pharyngogastropastie with left colonic interposition, due to severe oesophageal stricture after caustic ingestion.
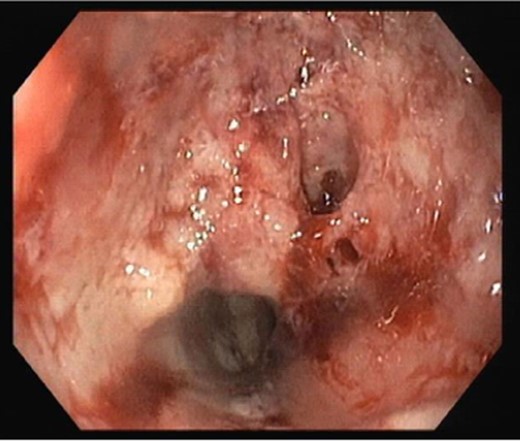
Upper digestive endoscopic study revealed an ulcerated vegetative neoplasia at 20 cm of the dental arch, insurmountable to endoscope (Fig. 1). A screening colonoscopy was unremarkable.
Laboratory investigation revealed normal carcinoembryonic antigen level, as well as cancer antigen 19.9.
Histologic examination revealed adenocarcinoma of colonic origin.
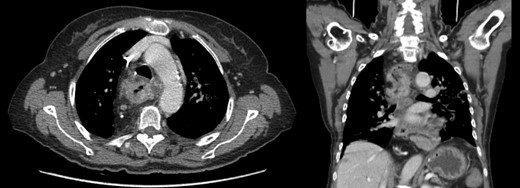
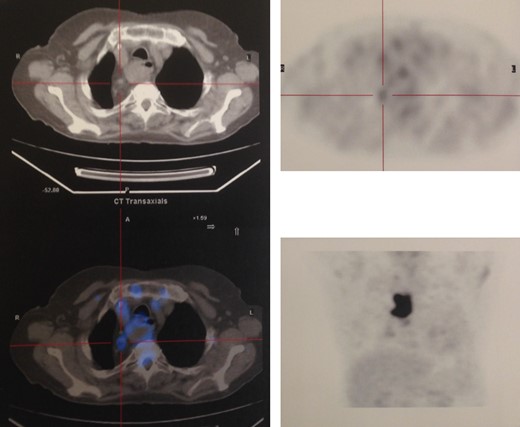
Staging with chest, abdomen and pelvic tomography, showed no signs of regional spread or metastatic disease (Fig. 2), and positron emission tomography scan revealed FDG (fluorodeoxyglucose) avidity in the primary lesion (retrosternal colic tube with thickened walls) and regional lymph nodes (Fig. 3).
The patient evolved to aphasia and, 1 month later, she was submitted to surgical gastrostomy.
The case was presented in a multidisciplinary meeting and she was proposed do neoadjuvant chemotherapy followed by removal of the colonic graft and definitive salivary fistula.
Re-stating after the sixth cycle of FOLFIRI and cetuximab (400 mg/m2) showed disease progression with enlargement of regional lymph nodes, and palliative chemotherapy was started.
The patient died 6 months after the initial diagnosis from severe respiratory failure caused by pulmonary thromboembolism.
DISCUSSION
Colonic interposition is an adequate oesophageal substitute, secondary to gastric pull-up, followed by jejunal graft, Roux-en-Y oesophagojejunostomy [4]. It is used to treat oesophageal injury due to trauma, stricture or cancer.
It is important to undergo colonoscopy before surgery to rule out pre-existing polyps, extensive diverticulosis and malignancy which are contra-indications for the interposition [1]. The left colon is preferred for the transposition due to its smaller diameter, but right colon or transverse colon interpositions are performed as well [5].
It carries perioperative mortality, and significant morbidity (including conduit ischemic injury, anastomotic leakage, vocal cord paralysis, stricture of the graft and ‘redundant graf’) [6].
Adenocarcinoma of the interposed colon is a rare occurrence, with <10 cases reported in literature (Table 1), and may be related to the irritation of colonic mucosa by gastric acid content or bile, occurring 5–47 years after surgery [4–10].
The published cases of adenocarcinoma of the colo-oesophagus after reconstruction for benign oesophageal strictures.
| Study . | Year of publication . | Sex, age . | Original disease . | Original treatment . | Years since reconstrution . |
|---|---|---|---|---|---|
| Licata et al. [10] | 1978 |
| Oesophageal stricture after corrosive injury | Right colon | 11 |
| Houghton et al. [8] | 1989 |
| Benign oesophageal stricture | Right colon | 20 |
| Altorjay et al. [10] | 1995 |
| Benign oesophageal stricture | Left colon | 5 |
| Hsieh et al. [10] | 2005 |
| Oesophageal stricture after corrosive injury | Right colon | 39 |
| Shersher et al. [4] | 2011 |
| Benign oesophageal stricture | Not specified | 40 |
| Kim et al. [9] | 2012 |
| Oesophageal stricture after corrosive injury | Right colon | 47 |
| Aryal et al. [1] | 2013 |
| Oesophageal stricture after corrosive injury | Right colon | 30 |
| Cheng et al. [10] | 2015 |
| Oesophageal stricture after corrosive injury | Right colon | 15 |
| Our report | 2018 |
| Oesophageal stricture after corrosive injury | Left colon | 19 |
| Study . | Year of publication . | Sex, age . | Original disease . | Original treatment . | Years since reconstrution . |
|---|---|---|---|---|---|
| Licata et al. [10] | 1978 |
| Oesophageal stricture after corrosive injury | Right colon | 11 |
| Houghton et al. [8] | 1989 |
| Benign oesophageal stricture | Right colon | 20 |
| Altorjay et al. [10] | 1995 |
| Benign oesophageal stricture | Left colon | 5 |
| Hsieh et al. [10] | 2005 |
| Oesophageal stricture after corrosive injury | Right colon | 39 |
| Shersher et al. [4] | 2011 |
| Benign oesophageal stricture | Not specified | 40 |
| Kim et al. [9] | 2012 |
| Oesophageal stricture after corrosive injury | Right colon | 47 |
| Aryal et al. [1] | 2013 |
| Oesophageal stricture after corrosive injury | Right colon | 30 |
| Cheng et al. [10] | 2015 |
| Oesophageal stricture after corrosive injury | Right colon | 15 |
| Our report | 2018 |
| Oesophageal stricture after corrosive injury | Left colon | 19 |
The published cases of adenocarcinoma of the colo-oesophagus after reconstruction for benign oesophageal strictures.
| Study . | Year of publication . | Sex, age . | Original disease . | Original treatment . | Years since reconstrution . |
|---|---|---|---|---|---|
| Licata et al. [10] | 1978 |
| Oesophageal stricture after corrosive injury | Right colon | 11 |
| Houghton et al. [8] | 1989 |
| Benign oesophageal stricture | Right colon | 20 |
| Altorjay et al. [10] | 1995 |
| Benign oesophageal stricture | Left colon | 5 |
| Hsieh et al. [10] | 2005 |
| Oesophageal stricture after corrosive injury | Right colon | 39 |
| Shersher et al. [4] | 2011 |
| Benign oesophageal stricture | Not specified | 40 |
| Kim et al. [9] | 2012 |
| Oesophageal stricture after corrosive injury | Right colon | 47 |
| Aryal et al. [1] | 2013 |
| Oesophageal stricture after corrosive injury | Right colon | 30 |
| Cheng et al. [10] | 2015 |
| Oesophageal stricture after corrosive injury | Right colon | 15 |
| Our report | 2018 |
| Oesophageal stricture after corrosive injury | Left colon | 19 |
| Study . | Year of publication . | Sex, age . | Original disease . | Original treatment . | Years since reconstrution . |
|---|---|---|---|---|---|
| Licata et al. [10] | 1978 |
| Oesophageal stricture after corrosive injury | Right colon | 11 |
| Houghton et al. [8] | 1989 |
| Benign oesophageal stricture | Right colon | 20 |
| Altorjay et al. [10] | 1995 |
| Benign oesophageal stricture | Left colon | 5 |
| Hsieh et al. [10] | 2005 |
| Oesophageal stricture after corrosive injury | Right colon | 39 |
| Shersher et al. [4] | 2011 |
| Benign oesophageal stricture | Not specified | 40 |
| Kim et al. [9] | 2012 |
| Oesophageal stricture after corrosive injury | Right colon | 47 |
| Aryal et al. [1] | 2013 |
| Oesophageal stricture after corrosive injury | Right colon | 30 |
| Cheng et al. [10] | 2015 |
| Oesophageal stricture after corrosive injury | Right colon | 15 |
| Our report | 2018 |
| Oesophageal stricture after corrosive injury | Left colon | 19 |
Most patients presented with dysphagia, but also with reflux related symptoms, and one case with respiratory infection [1, 4, 8–10]. The diagnosis and staging was made with upper gastrointestinal endoscopy, with biopsy consistent with adenocarcinoma of the colon, followed by CT scan and PET scan. In cases of interposed colonic carcinoma, further oncological treatment was considered base on the TNM classification. Resection of the interposed colon was the procedure of choice for cure.
Colon cancer in colon grafts should follow the age adjusted incidence rate. Although long-term risk analysis risk is lacking, it’s not unreasonable to propose endoscopic screening strategies, similar to general colonic cancer guidelines, in patients with colonic interposition grafts [1, 4, 10].
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- surgical complications
- deglutition disorders
- adenocarcinoma
- endoscopy
- constriction, pathologic
- esophageal stenosis
- esophagectomy
- risk assessment
- tissue transplants
- colon
- guidelines
- lymph nodes
- morbidity
- mortality
- colon cancer
- adenocarcinoma of colon
- caustic chemical ingestion
- esophageal reconstruction
- colonic interposition
- redundancy
- chemotherapy, neoadjuvant



