-
PDF
- Split View
-
Views
-
Cite
Cite
Egemen Tezcan, Rebecca Burrell, Daniel J Bell, Stefanos Almpanis, Spontaneous resolution of a spontaneous steinstrasse: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy252, https://doi.org/10.1093/jscr/rjy252
Close - Share Icon Share
Abstract
A 63-year-old man presented with a 4-day history of right sided loin-to-groin pain. Computed tomography imaging revealed a 22 mm by 7 mm volume of contiguous ureteric calculi at the right vesicoureteric junction. Spontaneous steinstrasse was diagnosed with no recent history of extracorporeal shock wave lithotripsy (ESWL) or other urological intervention to the right kidney. Metabolic testing was negative. An initial plan was made for urgent primary ureteroscopy and lithotripsy, however, the patient spontaneously passed 20–25 calculi at home whilst awaiting his operation date. He was reviewed in clinic and his symptoms had resolved. His ureteroscopy was cancelled. This case represents an example of spontaneous steinstrasse with no identified causative factors, a rare occurrence on which little literature is available presenting a management dilemma to the treating clinician. The case described resolved prior to intervention prompting us to suggest that spontaneous steinstrasse can be initially managed conservatively, as in ESWL-associated steinstrasse.
INTRODUCTION
Steinstrasse was the German term coined to describe the appearance of multiple ureterolithiasis observed as a complication of extracorporeal shock wave lithotripsy (ESWL) treatment in the late 1980s. Following fragmentation of a stone by ESWL, fragments passing down the ureter can stagnate leading to an accumulation of stones proximally. Cases of steinstrasse have also been described as complication of endoscopic lithotripsy and have been known to occur in patients with distal renal tubular acidosis [1]. Spontaneous steinstrasse with no identifiable precipitant is a rare phenomenon, described only in a few case reports over the years [2].
Post-ESWL steinstrasse can be asymptomatic, and conservative management has been demonstrated as being successful in around 50% of patients [3]. However, the steinstrasse can lead to pain, obstruction or sepsis leading to significant morbidity. Patients can present with flank pain, nausea and vomiting, symptoms of bladder irritation, or overtly septic with pyrexia [3]. Diagnosis may be made on different imaging modalities including X-ray, ultrasound, with increasing reliance on computed tomography (CT) scanning. Management options of steinstrasse that have been discussed in literature include a conservative approach, ESWL, ureteroscopy and very rarely open surgery [4].
CASE REPORT
A 63-year-old man presented with a 4-day history of right sided loin to groin pain. Non-contrast CT of the urinary tract (KUB) revealed multiple right distal ureteric calculi measuring 7 mm by 22 mm with mild dilatation of the right pelvicalyceal system (Fig. 1). There were multiple bilateral renal calculi, the largest measuring 7 mm. Urine culture revealed mixed growth. His renal function was not altered from baseline and electrolytes were unremarkable.
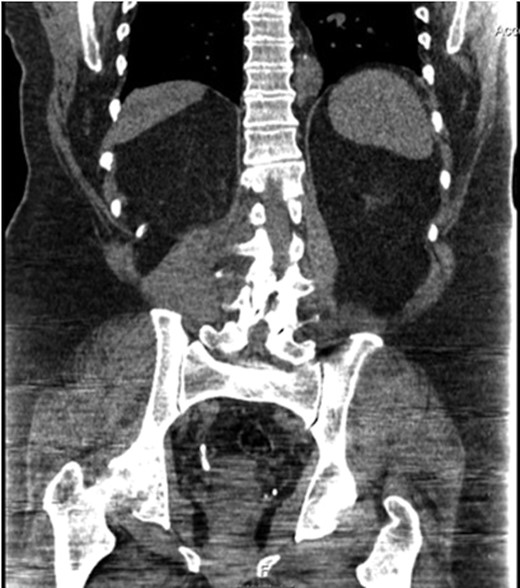
CT scan demonstrating contiguous right distal ureteric calculi measuring 7 mm by 22 mm.
His past medical history included previous renal stones bilaterally, hypertension, obesity, osteoarthritis and gout. In 2001 he was treated for left renal calculi, receiving initially ESWL treatment and subsequently percutaneous nephrolithotomy (PCNL) in 2005. Importantly, however, he had never had treatment on the right side which was now the side he was now symptomatic in.
He was discharged with Hyoscine Butylbromide (Buscopan), Diclofenac and Tamsulosin and was arranged to undergo a primary ureteroscopy and lithotripsy within 2 weeks. He subsequently presented to his pre-assessment appointment before surgery and explained that he had spontaneously passed 20–25 stones, of which he managed to keep 16 (Fig. 2). The stones measured between 2 mm smallest and 10 mm being the largest. On testing the calculi were determined to be calcium oxalate stones, the largest weighing 0.387 g. He was subsequently followed up in the Urology clinic, at which point his symptoms had resolved and his operation was cancelled.

Image of stones passed by patient measuring between 2 and 10 mm in length.
DISCUSSION
Steinstrasse is grouped into three types: type 1, multiple small fragments; type 2, a distal large fragment of >5 mm obstructing proximal small fragments; and type 3, multiple large fragments [3]. Conservative management of steinstrasse is successful ~50% of the time, however, only 10% of these patients have type 2 or 3 steinstrasse [3]. From the measurements of expelled stones of our case, we can comment that this could be classified as a type 2 or 3 steinstrasse.
It is, as ever, of utmost importance to take a detailed past medical history to identify any previous intervention or treatment for renal stones on the effected side. If any previous treatment has been performed then this may be a late or missed presentation of steinstrasse as a complication. This would be particularly relevant for patients who have not had sufficient follow up post-ESWL, with a long standing steinstrasse leading to renal damage potentially requiring a different approach to investigation and management.
This is a rare case of spontaneous steinstrasse with no history of treatment for renal stones on the effected side and no metabolic disorder such as renal tubular acidosis. ESWL has long been established as a safe and accessible treatment option for renal calculi, and ESWL-associated steinstrasse is a well recognized complication with a rich literature base to guide management. We know that overall 50–80% of post-ESWL steinstrasse cases resolve spontaneously [4], but we lack experience in managing spontaneous ones as they are rare. From all the available literature and our case the preliminary conclusion (level 4 of evidence) could be that the same management principles could apply for all steinstrasse cases regardless if they occurred spontaneously or post-ESWL. Improved knowledge and correct identification of spontaneous steinstrasse could avoid unnecessary intervention.
CONCLUSION
This case highlights the rare condition of spontaneous steinstrasse with no known causative factors. Such cases present a challenge to the treating clinician with regard to management decisions. In our case, the steinstrasse was passed spontaneously by the patient whilst awaiting elective intervention. Based on available literature and our case, we propose that similar to steinstrasse post-ESWL a trial of conservative management could result in resolution.
ACKNOWLEDGEMENTS
We would like the thank the patient involved for their permission to write up the case report.
CONFLICT OF INTEREST STATEMENT
No competing financial interests exist for any of the authors.



