-
PDF
- Split View
-
Views
-
Cite
Cite
Gabriel Alejandro Molina, Antonio Rolando Torres, Paul Sebastián Llerena, Alberto Yu, Andrea Carolina Sánchez, María Mercedes Cobo, Ascaris lumbricoides and its almost deadly complication, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy262, https://doi.org/10.1093/jscr/rjy262
Close - Share Icon Share
Abstract
Parasitic infections are still a burden in developing countries. The lack of sanitation and hygiene measures can result in an increase in morbidity and mortality due to parasitic infections. Surgery may be needed to treat serious complications caused by some of these parasites. Ascaris lumbricoides is one of the most common parasites and although infections are usually mild, severe complications, although rare, still exist. We present a case of a patient from the Ecuadorean Amazon region with limited access to drinking water. She presented to the emergency room with abdominal pain and a mass in the abdomen. After surgery, a mass with a perforation due to Ascaris was discovered. After discharge and due to lack of follow up and self-care, she became infected again, this time making her prognosis more complex and her clinical presentation more difficult. However, after proper clinical and surgical management, patient fully recovered.
INTRODUCTION
Parasitic infections can affect people of all ages and it has been associated to socioeconomic, environmental and sanitary-hygienic conditions [1]. Ascaris lumbricoides is a parasitic nematode and one of the most common parasites in the world [2, 3]. Infection can manifest with vomiting, malnourishment, pneumonitis, growth impairment and abdominal pain. If a severe infestation occurs, it can produce, cholangitis, pancreatitis, appendicitis or even masses with intestinal obstruction and in some rare cases, perforation [1, 2, 4, 5]. We report a case of a 55-year-old female who presented to the emergency room with abdominal tenderness and weight loss. After two surgeries the patient completely recovered. Bowel perforation due to Ascaris lumbricoides was the final diagnosis.
CASE REPORT
Patient is a 55-year-old female who presented to the emergency department with abdominal pain. She had been experiencing diffuse mild abdominal pain for the past year and reported that in the last 4 months the pain became more intense and was experiencing weight loss. On clinical examination, a dehydrated, malnourished and tachycardic patient with abdominal tenderness and a mass in the abdomen was discovered. She had leukocytosis with neutrophilia, and a heterogeneous mass with peripheral vascularity attached to the small bowel was revealed by echography. A contrast-enhanced CT confirmed a 10 × 11 × 5 cm3 mass in the transverse colon near the hepatic flexure that invaded the small bowel mesentery (Fig. 1A). The mass had a cavity filled with fluid and gas. Free abdominal fluid and some dilated loops of bowel were also observed (Fig. 1B). With these findings and after adequate resuscitation, surgery was decided. At laparotomy, 300 ml of purulent liquid in the abdominal cavity and a 10 × 10 × 5 cm3 blueish colonic mass, near the hepatic flexure that invaded the jejunum 50 cm distal to the ligament of Treitz, was discovered. Also, a 1 × 2 cm2 perforation was found in the mass from where fecaloid fluid poured into the abdomen. During surgery, an en-bloc resection of the colonic mass with the compromised jejunum was completed, the intestinal transit was restored with mechanical staples and an exhaustive washing of the abdominal cavity was done. Also, a drain was left near the colonic anastomosis. Pathology reported a 10 × 10 × 5 cm3 inflammatory colonic mass (Fig. 1C). The wall of the colon had necrotic patches (Fig. 2A). The jejunum wall had an inflammatory reaction that narrowed its lumen, nevertheless, no necrosis was found (Fig. 2B). The 3 × 3 × 2 cm3 cavity in the colonic mass contained purulent material and two adult Ascaris lumbricoides of 15 and 7 cm (Fig. 2C), one of which had multiple eggs in its uterine tubule (Fig. 3A). Beside this cavity, a 1 × 2 cm2 perforation was discovered. Bowel perforation due to roundworms, with colonic wall necrosis, was the final diagnosis.
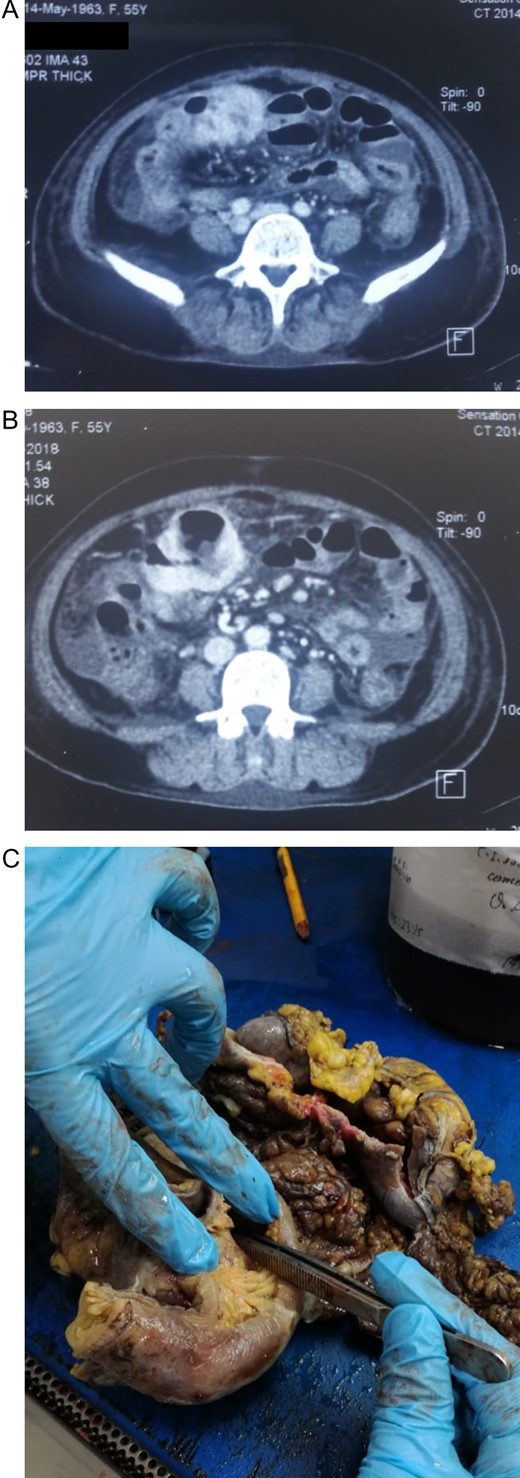
(A) CT revealing a mass in the colon that invaded the small bowel mesentery. (B) Colonic mass, with a cavity filled with fluid and gas. (C) Colonic mass and jejunum, colon with multiple ischemic and necrotic patches.
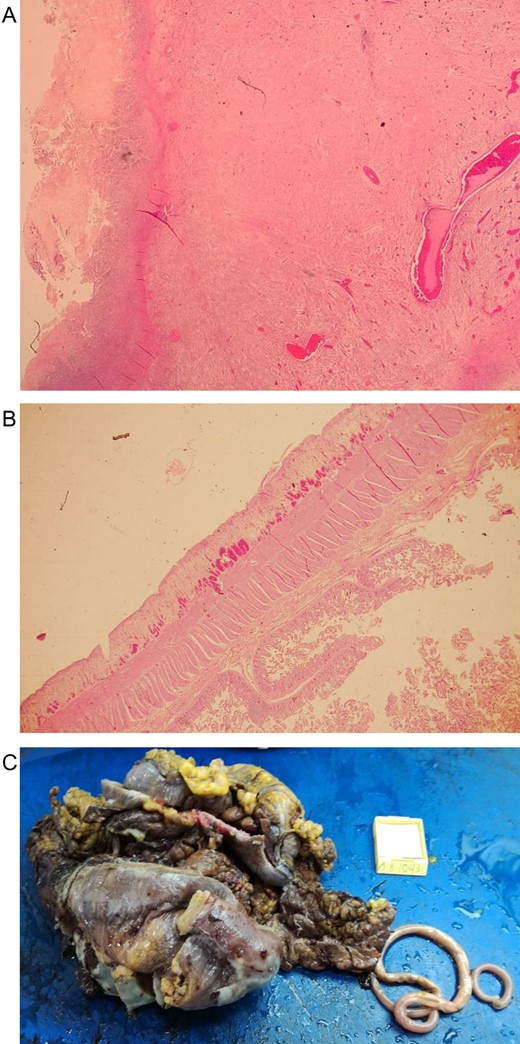
(A) Microscopic view of necrosis in the colonic wall. (B) Microscopic view of the inflammatory reaction in the jejunum wall. (C) Inflammatory colonic mass that compromised the jejunum with the two Ascaris.

(A) Female worms with multiples eggs in its uterine tubule. (B) Re-laparotomy with the enterocutaneous fistula managed like an ostomy. (C) Follow-up control, with adequate fistula management.
The postoperative period was uneventful, the patient was discharged after a 14-day antibiotic an anthelmintic treatment, and once full diet resumed. Nevertheless, 1 month later, she returned to the emergency with fever and abdominal pain. On clinical examination, abdominal tenderness and fecaloid fluid drained from the wound was discovered. Re-laparotomy was performed, a frozen abdomen with complete wound dehiscence was observed, the small bowel was matted together, covered in exudate, and had a granular appearance. An enterocutaneous fistula from the site of the colocolonic anastomosis from which feces drained and a live parasite emerged was unveiled. After extensive irrigation, the skin defect was closed, and the fistula was managed like wound ostomy in the midline (Fig. 3B). Following this surgery, patient had a good clinical development. Three months later on, follow-up controls patient is doing well (Fig. 3C).
DISCUSSION
Ascaris lumbricoides is a parasitic nematode and one of the most common parasites in the world, infecting 1.2 billion people globally [2, 3]. Infections are most common in the developing world [2], with higher prevalence among children [4]. In countries like Ecuador, where sanitary conditions are poor in some regions, people are at a higher risk of parasitic infections [6]. Our patient lives in the Amazon region with limited access to drinking water, which probably contributed to her infection. Ascariasis usually occurs by the ingestion of the embryonated eggs [3]. The larvae hatch in the small intestine and migrate to the colon where they penetrate its mucosa. Then, they reach the liver and advance to the lungs, where they cross the alveolar space and move to the pharynx. They are swallowed again and returned to the bowel where they can reach sexual maturity [2]. Ascariasis is influenced by lifestyle, socioeconomic factors and unhygienic defecation practices [2, 5, 7]. While the majority of infections are asymptomatic [4], 8–15% of those infected may present with varied gastrointestinal, pulmonary, and neurological symptoms. Although rare, life-threatening complications may present [1, 2], mainly associated with the presence of a large population of roundworms in the bowel [2].
Intestinal perforation due to Ascaris is controversial. It is thought that the parasite is simply a passenger within the intestinal Iumen and could only be able to escape into the peritoneal cavity through a preformed perforation caused by another enteric pathogen [8]. However, perforation of the terminal ileum and caecum due to Ascaris has been previously described [7]. The plasticity of the intestine allows the accumulation of many worms without any symptoms [3, 7]. Perforation may be due to roundworms pressing directly into the bowel wall in small spaces such as the appendix [3, 7], or through an inflammatory reaction [7, 9]. Diagnosis is based on the presence of adult worms or eggs in the stools [5]. Radiographs, ultrasound and CT are needed, especially when complications arise [9]. Ascariasis can be successfully treated with anthelmintic therapy. Surgery is rarely needed, however, when perforation is present, the type of surgery depends on the findings during laparotomy [3, 5].
In our patient, a perforated tumor was first suspected based on the clinical findings. However, the decision changed as the parasite was found. Even when at first the patient had good clinical development, the fact that she went back home to the same environment where she was first infected is likely to have changed her prognosis. Fortunately, she returned, and it was controlled.
This case illustrates how Ascariasis can develop into near fatal complications. Without adequate care and basic sanitary conditions, complications can become more severe. Cases like this call for a heightened awareness of the importance of good hygiene habits education especially in unattended areas of developing countries.
CONFLICT OF INTEREST STATEMENT
None declared.



