-
PDF
- Split View
-
Views
-
Cite
Cite
Christina Romero, Sandeep Sirsi, Armand Asarian, Jun Levine, Philip Xiao, Giant inflammatory polyposis, a phenomenon of inflammatory bowel disease, presenting as acute large bowel obstruction mimicking colonic neoplasm, Journal of Surgical Case Reports, Volume 2017, Issue 9, September 2017, rjx174, https://doi.org/10.1093/jscr/rjx174
Close - Share Icon Share
Abstract
Inflammatory bowel disease (IBD) remains a topic of ongoing research given its prevalence, yet the pathogenesis and all clinical manifestations of the disease remain poorly understood. Giant inflammatory polyposis is one of the clinical manifestations of IBD that has rarely been described to the best of our knowledge. This is a recognized clinical entity, however, only a limited number of IBD associated cases have been described in literature to date. This phenomenon consists of numerous benign, inflammatory polyps that clump together giving the appearance of a larger mass, which may cause clinical colonic obstruction and radiographic findings mimicking colonic neoplasm. This clinical entity may present in 10–20% of patients with IBD.
INTRODUCTION
Inflammatory polyps are relatively common in patients with inflammatory bowel disease (IBD), but the case we present of giant inflammatory polyposis (GIP) is not the same clinical entity. GIP is an uncommon manifestation of IBD that commonly consists of numerous filiform polyps that give an appearance of a ‘mass of worms’ or a ‘fungating’ mass. This clinical manifestation is also known as filiform polyposis, localized giant pseudopolyps, or just giant polyposis [1]. By definition the polyps are >1.5 cm in any dimension [2]. The proposed pathogenesis is that GIP is formed during the regenerative and healing process that leaves inflamed colonic mucosa in a polypoid configuration forming from residual islands of mucosa that remain after surrounding, severely inflamed mucosa becomes ulcerated [3, 4] Most of the reported cases have been located in the left colon: transverse colon (40%), sigmoid colon (15%), descending colon (15%), cecum (40%), splenic flexure (7%) and the hepatic flexure (7%) [5]. Symptoms from GIP can include but are not limited to anemia, cramping abdominal pain, melena, diarrhea, palpable mass, chronic mass with or without luminal obstruction and intussusception [1, 3, 4]. In the case we present, our patient had an obstructing mass in the transverse colon that manifested as cramping abdominal pain.
CASE REPORT
A 48-year-old African American male presented with localized, sharp and crampy right upper quadrant and left lower quadrant abdominal pain for 5 days associated with anorexia, nausea, vomiting, obstipation for 6 days and an unintentional 40 lb weight loss over the course of several months. The patient had history of hypertension, no known history of IBD or symptoms suggestive of IBD; however, he had a strong family history of Crohn’s disease.
On physical examination the patient was cachectic. The abdomen was soft, non-tender, non-distended, no guarding, no rebound tenderness, no rigidity. There was firm, immobile stool in the rectal vault without blood. Laboratory findings revealed hyponatremia and hypoalbuminemia, with otherwise normal laboratory values. CT scan on admission revealed transverse colon wall thickening with fecal impaction throughout the colon. Initial presentation was suspicious for malignancy, which prompted a colonoscopy on this same admission. There was a circumferential, polypoid, erythematous, friable mass like lesion with significant stenosis identified preventing endoscope progression.
Over the course of 12 days, the patient failed conservative management of large bowel obstruction, and subsequently underwent laparoscopic extended right hemi colectomy with primary anastomosis. On gross examination the transverse colon was firm, wall was thickened and proximal portion was severely dilated (Fig. 1). The specimen had massive inflammatory polyposis and colitis cystica profunda complicating idiopathic IBD, indeterminate type (Fig. 2). There was evidently continuous involvement of a long segment of the proximal colon with transmural chronic inflammation, fissuring ulcerations and chronic subserositis, which combined to produce mural thickening, rigidity and obstructive dilation of the cecum and ileum. Ileum was unremarkable. Microscopic examination the mass revealed colonic mucosa with extensive hyperplastic changes, mild active chronic colitis and crypt micro abscess without dysplasia (Fig. 3). The distal colonic margins demonstrated paneth cell metaplasia indicating IBD extends distally beyond the region of polyposis and may ultimately prove to be ulcerative colitis (UC).

Gross examination reveals thickened wall with portion of lumen dilation.
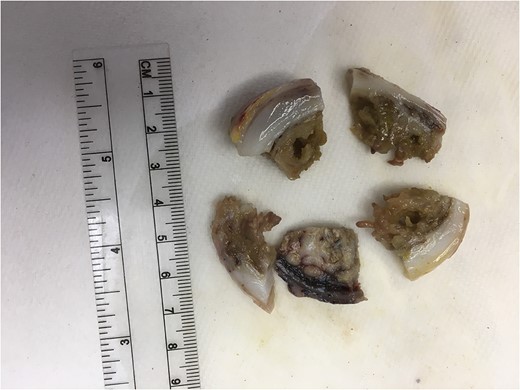
Gross examination reveals numerous polyps growing into the lumen.
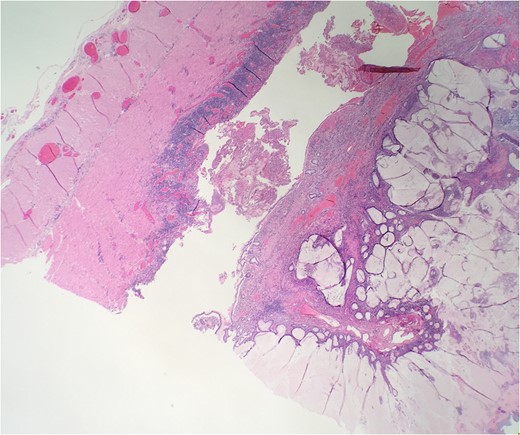
Microscopic examination reveals extensive hyperplastic changes with mucinous pool.
DISCUSSION
GIP occurs twice as often in UC compared to Crohn’s disease (CD) [2–4]. It often occurs adjacent to scarring and even transmural Crohn’s like inflammation may be seen. This mimicking of CD may be confusing to histopathologist; however, the diagnosis of CD cannot be made if the transmural inflammation is only in the area of polyposis [3]. Given our patient did not have a history of IBD prior to presentation, there was some question in regards to CD versus UC. Ultimately our patient’s working diagnosis is UC due to the fact that Paneth cell metaplasia extended beyond the region of polyposis, even though there was transmural inflammation in the region of polyposis. Keating and Mindell [6] reports that pseudopolyposis may be seen in either the active or quiescent state of UC. Given our patient’s lack of symptoms of IBD it supports the presence of GIP in the quiescent state. Because these can occur in the active and quiescent states, finding a GIP does not correlate with the severity of the underlying IBD [2]. Similar to a case reported by Syal et al., our patient’s first manifestation of IBD was GIP.
GIP totally obliterating the colonic lumen in a patient with UC was first reported by Fitterer et al. [5]. The case we present had GIP masquerading as an obstructing colonic mass in the transverse colon concerning for neoplasm. The major differential diagnosis for GIP is a polypoid colon adenocarcinoma, however, GIP is considered a benign entity. There has only been one reported case of an occult carcinoma arising in a patient who was diagnosed with localized GIP [5]. Although a diagnosis of GIP may be made correctly on the basis of radiology, endoscopy and histopathology, the possibility that a GIP hiding a carcinoma can never be excluded if the GIP is causing obstruction [3]. These inflammatory masses may appear worrisome because of their size, appearance and luminal obstruction. In essence, carcinoma associated with IBD often present as flat or depressed abnormalities and not as a protruded or pedunculated lesion [4]. The estimated incidence of a complicating malignancy in a patient with UC is 3–5%, suggesting that the risk of malignancy in a patient with UC and inflammatory polyposis is about equal to that in a patient without inflammatory polyposis [5].
In summary, we present this unique case of GIP presenting as colonic obstruction worrisome for colonic neoplasm as the first clinical manifestation of IBD. This is a clinical entity for surgeons, pathologist and gastroenterologist to be aware of. The management of these lesions is not well studied, but ultimately if the patient presents with obstruction like our case reported, it only seems logical that surgery would be indicated. The bigger question in our opinion is, the necessity for hemi colectomy versus segmental colonic resection of the portion involved given the low risk of malignancy.
CONFLICT OF INTEREST STATEMENT
None declared.



