-
PDF
- Split View
-
Views
-
Cite
Cite
Weronika Stupalkowska, Sarah F. Powell-Brett, Brandon Krijgsman, Grynfeltt-Lesshaft lumbar hernia: a rare cause of bowel obstruction misdiagnosed as a lipoma, Journal of Surgical Case Reports, Volume 2017, Issue 9, September 2017, rjx173, https://doi.org/10.1093/jscr/rjx173
Close - Share Icon Share
Abstract
Grynfeltt-Leschaft hernia is a type of lumbar hernia occurring in the superior lumbar triangle. Because of its rarity and non-specific presentation, lumbar hernia often poses a diagnostic challenge, and it can be easily misdiagnosed as a lipoma. If the correct diagnosis is missed, there is a significant risk of complications including hernia incarceration or strangulation. Here, we present a case of Grynfeltt-Lesshaft hernia which was repeatedly misdiagnosed as a lipoma and presented acutely with large bowel obstruction. A definite diagnosis was made by a computed tomography scan and the patient had emergency laparotomy and successful mesh repair of the hernia defect.
INTRODUCTION
There are only ~300 cases of lumbar hernias reported to date. Although rare, they are important to diagnose because of the significant risk of complications: 25% will become incarcerated and 8% strangulated [1]. Unfortunately, lumbar hernia is rarely included in a differential diagnosis of a flank swelling. Because of its rarity and non-specific presentation it can be easily confused with a lipoma. We present a case of Grynfeltt-Lesshaft hernia, misdiagnosed as a lipoma, causing large bowel obstruction and requiring an emergency laparotomy. This case highlights the importance of considering lumbar hernia in patients with flank swelling, and the potential complications from missing the correct diagnosis.
CASE REPORT
A 72-year-old woman presented with acute lower abdominal pain and nausea. She had not opened her bowels in 5 days and was passing no flatus. Her medical background included Parkinson’s Disease, hypothyroidism, hypertension, pulmonary embolism and deep vein thrombosis. Further history revealed a longstanding swelling in her left flank, diagnosed as a lipoma and excised 15 years ago under local anaesthetic. Interestingly, according to the patient, her swelling was unchanged after the procedure. A community ultrasound done over a year before her acute presentation had suggested the presence of a hernia (Fig. 1); however, the sonographer was not a musculoskeletal specialist and could not confirm the diagnosis. Biopsy only showed subcutaneous fatty tissue and the lump was diagnosed as a recurrent lipoma.
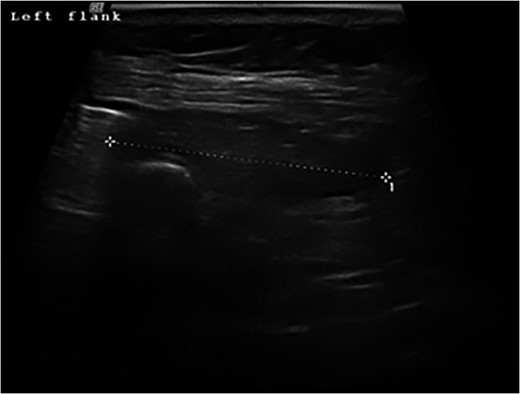
Ultrasound scan of the left flank showing possible hernia in a 72-year-old woman presenting with a flank swelling (dashed line).
On examination, there was a 15 cm, irreducible, mildly tender lump in the left superior lumbar triangle, in the region of previous lipoma excision. There were audible bowel sounds on auscultation of the lump. No other swellings of the abdominal wall were identified and the patient was not known to have any hernias. Abdominal radiograph revealed faecal loading in the ascending colon with dilated large bowel loops (Fig. 2). Subsequent computed tomography (CT) scan showed a left superior lumbar triangle hernia containing a loop of colon (Fig. 3) with dilated large bowel proximal to this, in keeping with obstruction.

Abdominal supine plain radiograph showing faecal loading in ascending colon and dilated large bowel loops in a 72-year-old woman diagnosed with large bowel obstruction secondary to left sided superior lumbar triangle hernia.
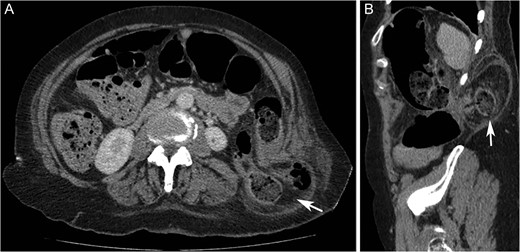
Computed tomography axial (A) and sagittal (B) images showing left sided superior lumbar triangle (Grynfeltt-Lesshaft) hernia containing loop of (‘arrows’) in a 72-year-old woman.
At emergency laparotomy a left-sided lumbar hernia with 2 × 3 cm defect was confirmed, containing necrotic omentum and a loop of descending colon. The left colon was mobilized lateral to medial and the hernia was reduced with external pressure by an assistant. Necrotic omentum was excised but the reduced bowel appeared healthy with no resection required. A retroperitoneal space was created and the hernia defect was repaired with 9 × 6 cm Prolene mesh placed in the plane between the opened peritoneum and the muscle. As it was not possible to completely close the peritoneum over the repair, a tongue of omentum was fixed between the repair and the descending colon.
Postoperatively, patient was supported in the intensive care unit but recovered well and was discharged on Day 9. Unfortunately, 1 month later she required second laparotomy and adhesiolysis for small bowel obstruction, with no signs of hernia recurrence or any involvement of the mesh in the adhesions. On review at 8 months, there was no evidence of hernia recurrence.
DISCUSSION
Anatomically, Grynfeltt-Lesshaft hernia occurs in the superior lumbar triangle, defined by the 12th rib, erector spinae muscles and posterior border of inferior oblique. It is more common that the Petit (inferior lumbar triangle) hernia.
The majority (55%) of lumbar hernias are primary (spontaneous) with predisposing factors such as old age, chronic lung disease, extremes of weight or muscular atrophy [2]. A further 20% are congenital and the remaining 25% are secondary (acquired)—resulting from trauma, surgery or infection [2]. In our case, it is likely that the patient developed a spontaneous lumbar hernia 15 years ago, incorrectly diagnosed as a lipoma.
Lumbar hernias most commonly contain omentum or colon but herniation of other organs such as small intestine, spleen or kidney has been reported [3–5]. Typically, these hernias present with lower back pain and flank swelling. Presentation with bowel obstruction, such as in this case, is rare, and includes only 9% of spontaneous lumbar hernias [2].
Because of its rarity and non-specific presentation, lumbar hernia can be easily confused with other pathologies that present as a superficial flank mass more commonly, for example lipomas [6, 7]. Clinical findings may be misleading as the overlying muscle and subcutaneous tissue can interfere with accurate examination [6].
In the vast majority of reported cases, including ours, a definite diagnosis was made on a CT scan. However, in our case, the presence of the hernia was suggested earlier, on an ultrasound. Potentially, if this had been investigated further at that time, the correct diagnosis could have been made earlier, avoiding the emergency admission with bowel obstruction and allowing for elective repair with a less invasive approach. Furthermore, it illustrates that ultrasound, if interpreted by appropriate specialists, can be used in diagnosis of lumbar hernias, as demonstrated before [8]. This might be of importance in specific situations like pregnancy, young age or in resource deprived areas.
Lumbar hernias tend to grow and become more symptomatic. Additionally, as mentioned earlier, there is associated morbidity. Therefore, the general consensus is that these hernias should be repaired surgically, unless patient is too high risk for an anaesthetic [2]. There are no established guidelines regarding the best technique for repair. For non-emergency cases both classic open and laparoscopic approaches have been used successfully [2]. However, in an emergency setting, when there is doubt about bowel viability, laparotomy has been reported [9]. This approach allows resection of non-viable bowel and adequate washout if required [9]. It does; however, increase the risk of certain complications such as adhesional bowel obstruction, as in this case.
In summary, our case demonstrates that lumbar hernia can be misdiagnosed as a lipoma: clinical examination, ultrasound and biopsy may all be inconclusive or misleading and a correct diagnosis commonly requires a CT scan. It is important not to miss a diagnosis of lumbar hernia as it is associated with significant morbidity, which can be reduced with early treatment. Therefore, diagnosis of a lumbar hernia should be considered in all patients presenting with a swelling in their flank, especially if thought to be a lipoma.
CONFLICT OF INTEREST STATEMENT
None declared.



