-
PDF
- Split View
-
Views
-
Cite
Cite
Kjetil Søreide, Andreas Reite, Rune Haaverstad, Missed diagnosis of a large, right-sided diaphragmatic rupture with herniated liver and concomitant liver laceration after blunt trauma: consequences for delayed surgical repair, Journal of Surgical Case Reports, Volume 2017, Issue 8, August 2017, rjx157, https://doi.org/10.1093/jscr/rjx157
Close - Share Icon Share
Abstract
Diaphragmatic injuries are relatively rare and as such frequently missed, particularly if they occur as a rare event on the right-sided dome. Even if detected in the early phase, the concomitant injury of other organs may delay the time to repair. The delay in surgical correction may aggravate additional adherences between thoracic and abdominal organs and cause the diaphragmatic muscle to retract, causing a larger tissue defect that may prevent primary suture repair. This should be taken into consideration when choosing access to repair (thoracic, abdominal or both cavities), mode (open or laparoscopic) and type of repair (primary suture or use of mesh material to close the defect). Here we present a case of delayed right-sided, blunt diaphragmatic injury with herniation of liver. Repair was performed in a delayed manner with an initial laparoscopic exploration converted to open abdominal repair with closing of defect with Gore-tex mesh material.
INTRODUCTION
Diaphragmatic injuries are relatively rare after blunt trauma and thus a relatively frequently missed diagnosis and subject to delayed surgery [1, 2]. Diaphragmatic injuries that occur in the right-sided hemidiaphragm are particularly prone to delayed diagnosis or even go undetected for years. The relatively infrequent occurrence in the right-sided diaphragm is related to the protective effect of the liver, compared to the left-sided diaphragm. For the same reason, these injuries may be hard to capture during the initial investigation and thus may present earliest on secondary or tertiary survey or, even in a delayed manner after years when the patient develops symptoms. Early diagnosis may facilitate repair before long-term effects occur, such as respiratory symptoms or reduced pulmonary capacity. In severe multitrauma, other injuries may initially dominate the clinical severity, hence, deviating the attention away from these injuries. Accordingly, a high degree of index suspicion is warranted to reduce the risk of missed diaphragmatic injuries, as delayed diagnosis or even missed injury may have major implications for both treatment and outcomes [3, 4].
CASE REPORT
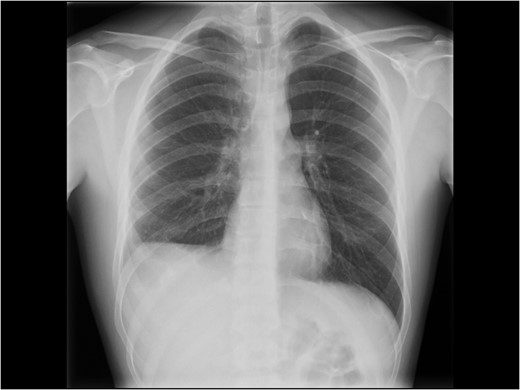
An adolescent male suffered a high-velocity fall while exercising ski-sports in the Alps. He suffered a severe blunt injury with temporary loss of consciousness and was brought to a local hospital where initial work-up and imaging showed no head injury other than a concussion, a right-sided pulmonary contusion with haematothorax and a grade II liver laceration involving segment 8. A right-sided chest drain was placed (Fig. 1) and was kept for several days with strict bed rest and monitoring under conservative management. After 14 days, he eventually was deemed fit for ground-ambulance transfer to our hospital. The chest drain was removed 4 days prior to departure.
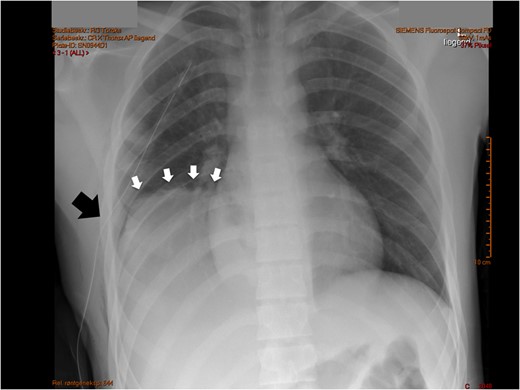
Initial chest X-ray after placement of thoracic drain. White arrows note a high-stand of the right diaphragm, black arrow points to chest drain.
On admission after transfer to our hospital he had stable vital signs, with none or little complaints or symptoms. The transferred radiological images from the primary hospital were reviewed and gave immediately suspicion of additional pathology in the right hemithorax, based on a prominent right-sided high-stand of the diaphragm (Fig. 1). A CT scan was made showing a grade II liver laceration and a herniated liver through a large right-sided defect of the right diaphragm (Fig. 2A and B).
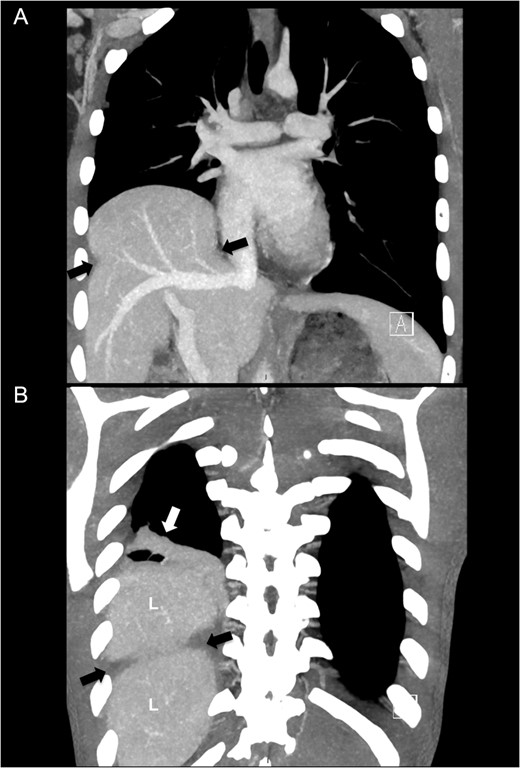
Computed tomography of right-sided diaphragm rupture and herniated liver. (A) CT performed after transfer showing ruptured diaphragm (black arrows) with herniated liver into the right thoracic cavity. (B) A more posterior view with pulmonary atelectasis (white arrow). L denotes liver.
Due to the delayed presentation and concomitant presence of a subacute liver injury with fragile tissue, the decision to delay elective treatment of the diaphragm was made. The patient was admitted 8 weeks later for elective repair. An initial laparoscopic approach was attempted, but was converted to open repair by an inverse L subcostal incision due to the size of the defect and adhesions of diaphragmatic edges on surfaces to the liver. In addition there were pulmonary adhesions to the posterior liver surface (Fig. 3A). Adhesiolysis was performed of the diaphragmatic defect to the liver. A double lumen ventilation tube allowed for deflating of the right lung and gentle dissection of the pulmonary adhesions to the liver. Considerable loss of tissue domain of the diaphragm due to retraction and fibrosis was noted (Fig. 3B) for a grade V diaphragm injury (Table 1) based on the AAST score [5]. The size of the defect, measured as 10 cm × 5 cm (50 cm2) prevented primary suture repair of the diaphragm in an end-to-end fashion. Thus, a 1 mm thick Gore-Tex™ patch was used to cover the defect (Fig. 2A) and a pulmonary drain was placed (Fig. 4B). The patient recovered uneventfully, the chest drain was removed on post-operative Day 2 and he was discharged on post-operative Day 6 with a recommendation not to resume full physical activity until 2 months after surgery. When he was seen in the outpatient clinics 3 months later postoperatively, he had resumed full physical activity including sports. He had no complaints and had a well-healed scar. An erect chest X-ray showed a moderately high-standing diaphragm on the right side (Fig. 5).
| Grade . | Injury description . |
|---|---|
| I | Contusion |
| II | Laceration ≤2 cm |
| III | Laceration 2–10 cm |
| IV | Laceration >10 cm with tissue loss ≤25 cm2 |
| V | Laceration with tissue loss >25 cm2 |
| Grade . | Injury description . |
|---|---|
| I | Contusion |
| II | Laceration ≤2 cm |
| III | Laceration 2–10 cm |
| IV | Laceration >10 cm with tissue loss ≤25 cm2 |
| V | Laceration with tissue loss >25 cm2 |
After Moore et al. [5].
| Grade . | Injury description . |
|---|---|
| I | Contusion |
| II | Laceration ≤2 cm |
| III | Laceration 2–10 cm |
| IV | Laceration >10 cm with tissue loss ≤25 cm2 |
| V | Laceration with tissue loss >25 cm2 |
| Grade . | Injury description . |
|---|---|
| I | Contusion |
| II | Laceration ≤2 cm |
| III | Laceration 2–10 cm |
| IV | Laceration >10 cm with tissue loss ≤25 cm2 |
| V | Laceration with tissue loss >25 cm2 |
After Moore et al. [5].
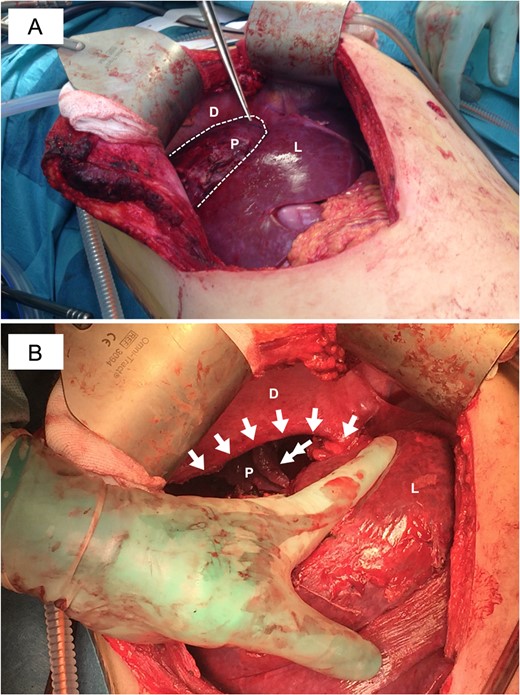
Intraoperative view of the diaphragmatic injury. (A) View showing the diaphragm (D) with the defect illustrated by dotted line and the pulmonary (P) tissue adhered to the liver (L) surface. (B) After dissection of adhesions and release of the lung (P) the defect was measured to ~10 cm in the mediolateral extension (extending almost at the insertion of the right hepatic vein to the lateral part of the diaphragmatic dome) and ~5 cm in the anterioposterior direction.
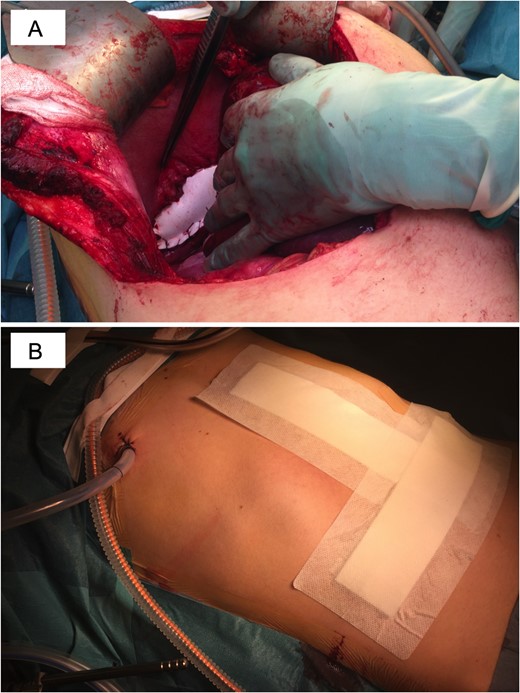
Surgical repair of diaphragmatic defect using a Gore-tex mesh. (A) A polytetrafluoroethylene mesh (Gore-Tex™) was sutured to cover the defect. (B) A chest drain was placed and kept for 3 days.
Chest X-ray at follow-up. Still some degree of diaphragm high-stand on the right side.
DISCUSSION
Blunt traumatic diaphragmatic injuries are rare and easily missed on initial diagnosis. Diaphragmatic injuries may be seen in as few as 0.06% of all blunt trauma patients based on an Israeli series [6]. Data from the National Trauma Databank in the USA suggest an occurrence of 0.46% of all trauma, but two-thirds of the injuries were from penetrating trauma, thus leaving blunt mechanism as the cause of 0.15% of all diaphragmatic injuries [7]. An early and accurate diagnosis of diaphragmatic injury in the setting of blunt and penetrating trauma can be difficult even with the help of sophisticated diagnostic modalities [1]. Computed tomography is the mainstay in the diagnosis of such injuries, which may be subtle at presentation. Key features in blunt trauma include diaphragm fragment distraction and organ herniation because of increased intra-abdominal pressure [8]. Right-sided diaphragmatic injuries occur less frequent than left-sided, and about one-third of injuries are associated with a hematothorax [9]. Right-sided lesions are also much more frequently missed and thus may present with late symptoms.
The current patient was diagnosed after transfer to our hospital, with diagnosis missed on initial receipt and care at the receiving institution. As he was asymptomatic and had a concomitant liver laceration, the repair was delayed. One may in theory consider this to have caused the defect to additionally increase in size and adhesions to be more dense, potentially causing a grade III tear to develop into of a grade V injury with larger defect due to retraction of tissue. This should be taken into consideration when choosing the treatment options. A thoracic or abdominal approach has been described with no major differences in outcomes, and likely reflecting a convenience choice for the surgeon in terms of access route. Laparoscopic repair is described in may case reports and case series, but its success is partly dependent on timing of surgery, as adhesions and larger defects are less likely to be feasible for laparoscopic repair. The current case needed coverage of a large defect with several adhesions to pulmonary tissue, thus an open approach was felt to be the safest and most effective mode of repair. Outcome in the short-term (<1 year after surgery) was good, with resumption of normal physical and sports activity.
CONFLICT OF INTEREST STATEMENT
None declared.



