-
PDF
- Split View
-
Views
-
Cite
Cite
Sunday J Lengmang, Abubakar B. Dakingari, Paul Ushie, George A.A. Chima, Edwin Oseni-Momudu, Ureterovaginal fistula following spontaneous vaginal delivery, repaired by vaginal ureteroneocystostomy in a low resource setting, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx143, https://doi.org/10.1093/jscr/rjx143
Close - Share Icon Share
Abstract
Ureterovaginal fistula commonly follows ureteric injury during pelvic surgery, and presents with continuous urinary incontinence in spite of normal micturition. Continuous urinary incontinence has significant impact on quality of life, thus requiring effective surgical intervention in order to restore health. We found no reported case of ureterovaginal fistula following spontaneous vaginal delivery with prolonged obstructed labour. Relevant history and simple diagnostic procedures were used for diagnosis and the patient had successful vaginal ureteroneocystostomy. This could be the first reported ureterovaginal fistula following spontaneous vaginal delivery with prolonged obstructed labour. Vaginal ureteroneocystostomy though scarcely reported, is feasible in selected cases.
INTRODUCTION
Ureterovaginal fistula is mainly iatrogenic, and commonly complicates pelvic surgeries [1, 2]. Ureteral injuries occur in 0.5–2.5% of gynaecological surgeries [1, 2]. Whereas studies from low resource settings have reported a higher proportion of ureterovaginal fistula complicating caesarean deliveries [3], the scenario in other countries reveal higher proportions following hysterectomy [1, 3]. In a recent review of the aetiology of ureterovaginal fistula, only one case was associated with uterine rupture complicating vaginal delivery [1]. We found no case of ureterovaginal fistula following spontaneous vaginal delivery with prolonged obstructed labour in published literature.
Ureterovaginal fistula presents with constant incontinence of urine with devastating physical, social and mental consequences; and significantly impacts the quality of life [4]. It is therefore imperative that women suffering from this devastating disease be offered immediate and effective care to alleviate their suffering.
The care offered to women with ureterovaginal fistula varies significantly depending on availability of resources. The medical literature offers different approaches to the diagnosis of ureterovaginal fistula. Surgical options and preferences also vary. This case emphasizes the scenario in low resource settings which are equally effective but scantly reported in the medical literature.
CASE
A 20-year-old Para 1 woman presented with continuous urinary incontinence in spite of normal micturition for one month. Her symptoms followed an unsupervised spontaneous vaginal delivery which lasted for more than 24 h, resulting in foetal demise. The pregnancy and delivery was not attended by a skilled birth attendant and there was no instrumentation during delivery.
Direct dye test using 300 ml of dilute methylene blue instilled into the bladder showed no dye leak. However, a clear stream of urine was seen spilling from the left ureter (Fig. 1). The ureter was catheterized with a ureteral catheter for up to 6 cm. Furthermore, a three swab test confirmed ureterovaginal fistula as the swab near the cervix was soaked with urine but the other swabs were neither dye-stained nor soaked. The diagnosis of left ureterovaginal fistula was made and the patient was prepared for surgery. Her packed cell volume was 34%; HIV was non-reactive; while urea and creatinine were within normal limits.

Direct dye test: 300 ml methylene blue instilled into the bladder through Foley catheter shows no dye leak, but a clear stream of urine spilling from the left ureter.
The diagnosis and treatment options were discussed with the patient and she signed an informed consent for left ureteroneocystostomy by vaginal approach.
Ureteroneocystostomy was done via the vaginal route under spinal anaesthesia. An inverted ‘T’ shaped incision was made at the distal border of the left ureter, and the anterior vaginal wall was dissected, taking care to free the distal left ureter over the ureteral catheter. An artery clamp was passed through the urethra and used to pierce the bladder, creating a tiny bladder fistula around the distal margin of the left ureter through which the ureteral catheter was pulled through the bladder and out through the external urethral meatus. The ureter was then reimplanted into the bladder using 4/0 Vicryl at four quadrants by passing each suture from the serosal margin of the distal ureter exiting through the mucosa and then through the mucosa of the bladder exiting the bladder serosa. A second layer of bladder serosa was closed over the reimplanted ureter using Vicryl 2/0 (Fig. 2). The urethra was catheterized and post closure dye test was negative, so the vaginal wall was closed with vicryl 2/0 in one layer (Fig. 3).
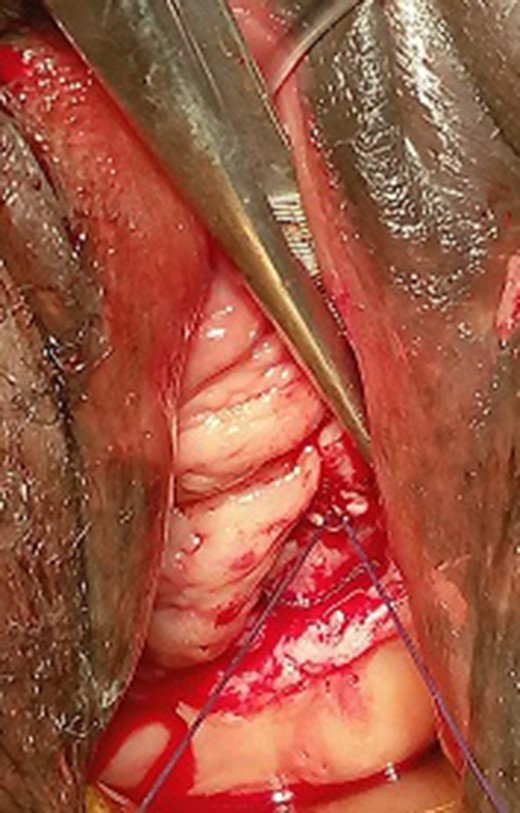
Bladder closed over left reimplanted ureter, with ureteral catheter exiting the external urethral meatus.
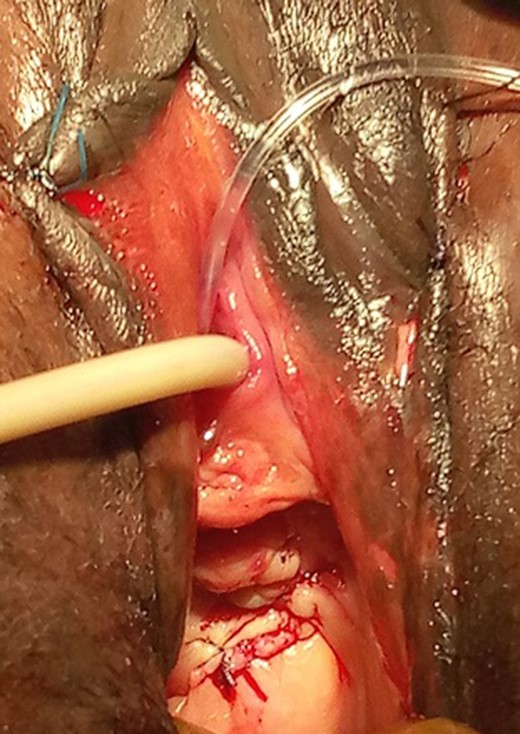
Anterior vaginal wall closure with ureteral and urethral catheters exiting from the external urethral meatus.
The patient had an uneventful recovery and post-operative period, and the catheters were removed after 14 days. The patient was completely continent of urine at discharge and remained continent at last follow up 2 years thereafter.
The patient was therefore discharged from follow up after repeated sessions of counselling for prenatal planning, antenatal care and supervised delivery in a hospital to ensure safe subsequent deliveries.
DISCUSSION
Prolonged obstructed labour, home delivery and foetal loss are common findings in women with genital fistula in low-resource countries. Pressure necrosis often follows prolonged obstructed labour and results to fistula formation. The direct opening of the left ureter to the vagina in this case suggests pressure necrosis and sloughing of the anterior vaginal wall as possible cause for the fistula.
The history of urinary incontinence in spite of intermittent normal voiding of urine suggested one ureter bypassing the bladder into the vagina while the other remains normally placed in the bladder. The direct dye test supported the diagnosis of ureterovaginal fistula, since dye placed into the bladder did not leak to the vagina; implying normal integrity of the bladder. Ureterovaginal fistula was confirmed when urine was seen spilling directly from the ureter into the vagina. Further confirmation was made with the three swab test. These steps appear to be sufficient for most diagnoses of ureterovaginal fistula in low resource settings, where most patients presenting with urogenital fistula are indigent [3]. Most childbirth injuries in low resource settings affect the poorest of the poor who would otherwise endure the scourge of fistula for life, except if surgery was highly subsidized or offered at no cost to the patient. Conversely, abdominal ultrasound, CT scan, cystoscopy, intravenous pyelography, retrogate pyelography, vaginogram, cystogram and voiding cystometry are commonly used in different combinations where resources are available [1].
Conservative minimal invasive treatment with JJ Stent for 6–8 weeks is possible [4], but Memokath stent with extended period offered a better outcome [3]. Failed ureteral stenting is treated by ureteroneocystostomy by open, laparoscopic or robotic abdominal approach [4].
Ureterovaginal fistulae in low resource settings are commonly operated by open abdominal ureteric reimplantation. In our experience, reimplantation by the abdominal route is best fit for women whose ureterovaginal fistula complicated pelvic surgery where the ureter is often ligated along with bleeding vessels. However, since this case followed a spontaneous vaginal delivery; the ureteral opening into the vagina could readily be seen and catheterized for up to 6 cm, we offered ureteroneocystostomy through the vaginal route as was the experience of others [4]. This approach has the advantage of being extraperitoneal, minimally invasive [4] and leaves no obvious scar.
Our patient had an uneventful post-operative period with the ureter and urethra catheterized for 2 weeks with a successful outcome. Others have catheterized the ureter for three weeks [3]. Shorter catheterization appears to offer significant advantages in clinical care and programming. It could reduce urine tract infection, increase turnover with opportunity for more patients to be operated especially when bed space is limited.
Since our patient's first delivery had a poor outcome (ureterovaginal fistula and foetal demise), it is important that subsequent pregnancies be closely monitored, and deliveries be attended by trained healthcare providers. Furthermore, it is advisable that subsequent deliveries be by caeserean section, as they often produce bigger babies which could further increase the risk of recurrent obstetric fistula.
Spontaneous vaginal delivery does not exclude diagnosis of ureterovaginal fistula, as this case demonstrates that ureterovaginal fistula could result from ureteric injury following spontaneous vaginal delivery with prolonged obstructed labour. Simple diagnostic procedures like direct dye and three swab tests are often sufficient for diagnosis of ureterovaginal fistula in low resource settings. Vaginal ureteroneocystostomy is an effective minimally invasive extraperitoneal option in selected cases.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Fistula Foundation USA provides funding for patient care.



