-
PDF
- Split View
-
Views
-
Cite
Cite
Salahoudine Idrissa, Mohamed Tazi, Hind Cherrabi, Abdoulaziz Souley, Abdelhalim Mahmoudi, Aziz Elmadi, Khalid Khattala, Youssef Bouabdallah, Multifocal rib osteomyelitis in children: a case report and literature review, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx142, https://doi.org/10.1093/jscr/rjx142
Close - Share Icon Share
Abstract
Rib osteomyelitis is a rare disease, occurring in ~1% or less of all cases of haematogenous osteomyelitis. During the last century, 58 cases of rib osteomyelitis were reported in the literature, of which, multiple ribs were involved in only five patients. Because of its rarity and non-specific clinical signs, diagnostic of rib osteomyelitis may be delayed. We report a case of multifocal rib osteomyelitis revealed by a dorsal mass in a healthy 13-year-old female child.
INTRODUCTION
Osteomyelitis is one of the most common invasive bacterial infections in children leading to hospitalization and prolonged antibiotic administration [1]. In industrialized countries, acute osteomyelitis occurs in ~8 of 100 000 children per year, but it is considerably more common in low-income countries [2]. Most cases of osteomyelitis in children arise in the metaphysis of long bones, such as femur, tibia and humerus [1]. Involvement of short and flat bones such as ribs, are extremely rare. To our knowledge only 58 cases of rib osteomyelitis were reported in the literature. In most children, the rib osteomyelitis presents with fever accompanied by a mass in the chest, near the costochondral junction or near the costovertebral angle [3]. But sometimes, local signs and symptoms are mild and may delay diagnosis and appropriate management. We report a case of multifocal rib osteomyelitis revealed by a dorsal mass of the chest wall in a 13-year-old female child.
CASE REPORT
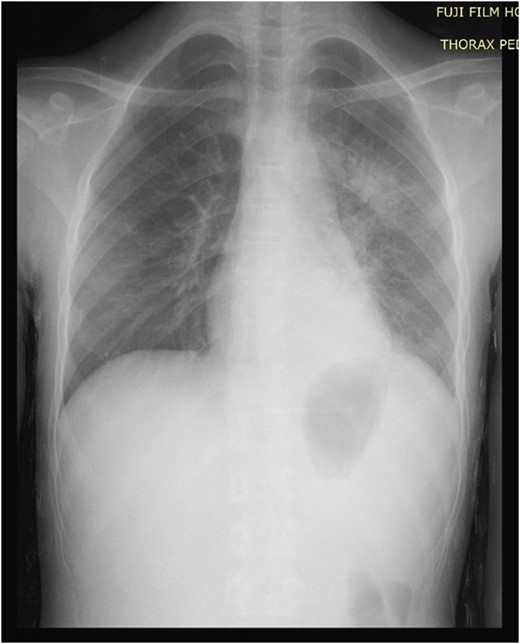
A 13-year-old female child was presented to the pediatric emergency unit with a painful swelling of the posterior left chest wall during the last 3 months. The patient was febrile without weight loss. She had a history of cutaneous mycosis for 2 years. The physical examination revealed a child in good general condition, febrile (axillary temperature was 38.2°C) and a painful swelling of the left posterior chest wall of ~6 × 4 cm2 (Fig. 1). The laboratory studies found a hemoglobin and hematocrit level of 10.5 g/dL and 34.4%, respectively, and a white blood cell count (WBC) of 15.210/μL with 80% neutrophils. Inflammatory indices such as erythrocyte sedimentation rate and C-reactive protein were greatly increased, with a level of 50 mm/h and 111 mg/L, respectively. The chest and the abdominal radiographs were found to be normal (Fig 2). The ultrasound showed an echogenic collection of the posterior chest wall of ~5 cm × 5 cm. A computed tomography (CT) scan of the chest with intravenous (IV) contrast showed a 6-3-5 cm pus collection of the posterior costovertebral region consistent with an osteomyelitis of the 10th, 11th, 12th ribs and soft tissue collection (Fig. 3). The abscess was incised and drained. A rib biopsy and a cytological examination of the pus were performed. Postoperatively the abscess was drained by a chest tube for two days before being removed. Postoperative antibiotic therapy with ceftriaxone, gentamicin and metronidazole was initiated. The pus culture was negative. Mantoux test and HIV test were negative. The histological examination of the rib biopsy disclosed a diagnosis of acute non-specific rib osteomyelitis. The patient was discharged after 2 weeks from hospital and the injection antibiotics were switched to oral administration (amoxicillin-acid clavulanic 80 mg/kg/day) for 6 supplementary weeks. The patient remains asymptomatic 6 months postoperatively.

Physical examination: a swelling of the left posterior chest wall of ~6 × 4 cm2.
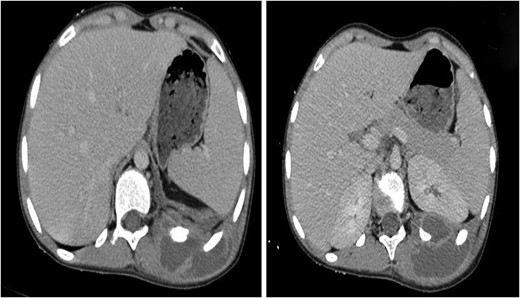
Soft tissue and bone windows of a chest CT scan show a 6-3-5 cm pus collection of posterior chest wall. The mass appeared to traverse kidney capsule and the thoracic cage to be continuous with a pleural-based mass adjacent to it.
DISCUSSION
We initiated our research by reviewing the references as published in PubMed (http://www.ncbi.nlm.nih.gov/pubmed), from 1916 to 2016 using the key words: osteomyelitis and rib, in subjects between 0 and 18 years of age. During the last century, 58 cases of rib osteomyelitis were reported in the literature, of which, multiple ribs were involved in only five patients. Rib osteomyelitis is a rare disease that occurs in ~1% or less of all osteomyelitis [4]. It can result from direct inoculation from traumatic wounds, by spreading from adjacent tissue affected by cellulitis or septic arthritis, or through hematogenous seeding. In ribs, as in long bones, hematogenous disease occurs in areas with the largest blood supply where the bone is more metabolically active. Those favored sites for dissemination are: anteriorly, near the costochondral junction (76%), and posteriorly, near the costovertebral angle [5]. The usual clinical presentation of rib osteomyelitis is a patient with fevers accompanied by an abscess or draining sinus that fails to heal [6]. Staphylococcus aureus is by far the most common causative agent in osteomyelitis [2]. This is not what happens in the developing world where rib osteomyelitis is frequently due to Mycobacterium tuberculosis [3]. Fungal infections are also a significant cause of rib osteomyelitis [7], although they occur frequently as part of multisystem-disseminated disease in immunocompromised patients. We are unaware of the genesis of the infection in our patient, but the fact that she had been treated for cutaneous mycosis for 2 years is an interesting argument not only for the gateway but also for the cause, especially with the frequency of fungal rib osteomyelitis. From a differential diagnosis point of view, the Ewing sarcoma was been suspected, but a normal chest wall X-ray eliminates this diagnosis. The routine chest X-rays sometimes failed to detect early skeletal disease and the diagnosis was often delayed until there was bone destruction with overlying soft tissue changes [8]. The early change of rib osteomyelitis that will appear usually 1–2 weeks later, is pericostal edema demonstrated by soft tissue swelling of the thoracic wall accompanied by an adjacent inward pleural displacement [9]. Pericostal edema can be readily diagnosed by ultrasound. A CT scan can be useful, but magnetic resonance imaging is the key exam for diagnosis in acute hematogenous osteomyelitis. It especially identifies marrow edema that is apparent in the early phases of metaphyseal infection before other imaging modalities are diagnosed [10]. However the definitive diagnosis of rib osteomyelitis requires a culture of the aspirated metaphysis or subperiosteal pus or blood cultures [5]. The surgical treatment consists of incision and drainage of the abscess with intraoperative wound culture. Postoperatively, the patient should be treated with a course of IV antibiotics with Gram-positive organism coverage [6].
In conclusion, rib osteomyelitis in children, although rare, has been reported. It can be easily misdiagnosed because of its rarity and non-specific clinical signs. Clinicians should be aware of the possibility of rib osteomyelitis in children that present a fever accompanied by a painful swelling near the costochondral junction or near the costovertebral angle.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to declare.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
ACKNOWLEDGMENTS
The authors thank the patient and her parents for allowing us to publish this case report.



