-
PDF
- Split View
-
Views
-
Cite
Cite
Nolan Mann, Truong Ma, Arthur Dalton, Neurofibromatosis type 1 and male breast cancer: emerging risk factor?, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjw138, https://doi.org/10.1093/jscr/rjw138
Close - Share Icon Share
Abstract
Neurofibromatosis type 1 (NF1) is an autosomal dominant disorder characterized by the appearance of cafe au lait spots, neurofibromas and Lisch nodules. There is an established link between NF1 and the development of breast cancer in women; however, due to the rarity of both NF1 and male breast cancer, the same link has yet to be elucidated in men. The concurrent presentation of NF1 and male breast cancer is a very rare phenomenon with only a handful of case descriptions in the literature. To the best of our knowledge, there have only been four other reported cases of NF1 and male breast cancer before ours. We present one such case of a 56-year-old male with a four generation history of NF1 and a personal history of NF1 who presented with invasive ductal carcinoma of the right breast.
INTRODUCTION
Neurofibromatosis type 1 (NF1), is an autosomal dominant genetic disorder with variable expressivity, with an estimated incidence of 1 in 3000 [1]. This disease is characterized by changes in skin coloration and the development of tumors along nerves in the skin, brain and various other regions of the body. The vast majority of persons affected will develop the characteristic cafe au lait spots and skin fold freckling early on in childhood, Lisch nodules in the iris and a delayed acquisition of neurofibromas in adulthood [1]. The disease is caused by a microdeletion of a gene located on Chromosome 17, which normally encodes for a protein known as neurofibromin. Neurofibromin is a negative regulator of the Ras oncogene pathway, and when disrupted, places the individual at a 4-fold increased risk of the development of malignancy compared to the general population. Those with NF1 are at increased risk for a variety of cancers, including, optic gliomas, peripheral nerve sheath tumors, pheochromocytoma, rhabdomyosarcoma, schwannoma, carcinoid tumors and so forth. There has been little data regarding the risk of more commonly occurring cancers (breast, colon and lung) in the NF1 population. While the relationship between NF1 and breast cancer in women is well established, to the best of our knowledge, there have only been four reported cases of breast cancer development in male patients with NF1 [2–4].
CASE DESCRIPTION
A 56-year-old male presented with a right-sided breast mass confirmed on mammogram as a 5.4 × 4.4 cm lobulated solid mass suspicious for cancer (Fig. 1). Axillary ultrasound revealed one suspicious lymph node. Core needle biopsy of the breast mass showed invasive poorly differentiated ductal carcinoma, ER+/PR+/HER+. The lymph node biopsy was negative for malignancy. Medical history was significant for hypertension and neurofibromatosis type 1. The patient noted no family history of breast, ovarian or prostate cancer; however, there was a four generation history of neurofibromatosis on his mother's side.
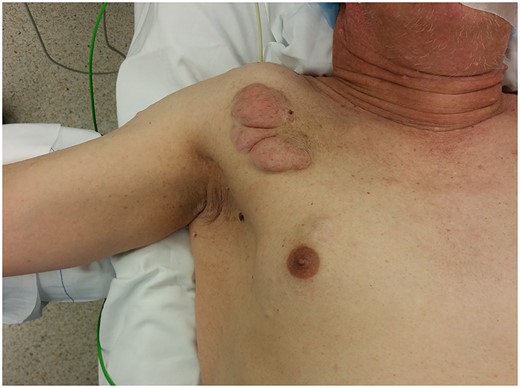
Right chest wall neurofibroma. Breast cancer is superior to the nipple.
Staging positron emission tomography computed tomography (PET CT) was performed demonstrating activity in the right breast as well as mediastinal and hilar lymphadenopathy (Fig. 2). The patient underwent neoadjuvant chemotherapy and a repeat PET CT showed decreased activity in the right breast and no further lymphadenopathy (Fig. 3). A right modified radical mastectomy was performed. Pathologic examination revealed invasive ductal carcinoma, histologic grade III with closest margin at 1mm away. There was 0 out of 18 positive axillary lymph nodes. Pathologic staging was set at pT2N0M0, Stage IIA. Given the slim posterior margin, he received post mastectomy radiation therapy. Currently, the patient is receiving tamoxifen 20 mg once a day.
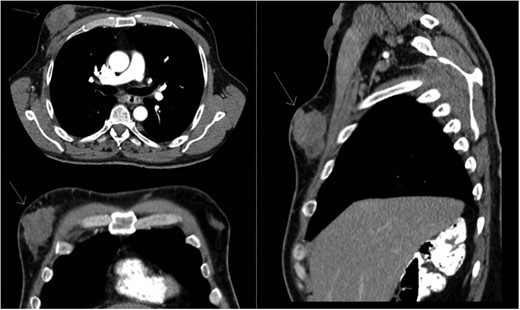
Preoperative staging CT scan. Chest wall mass noted to be 6.9 cm × 2 cm.
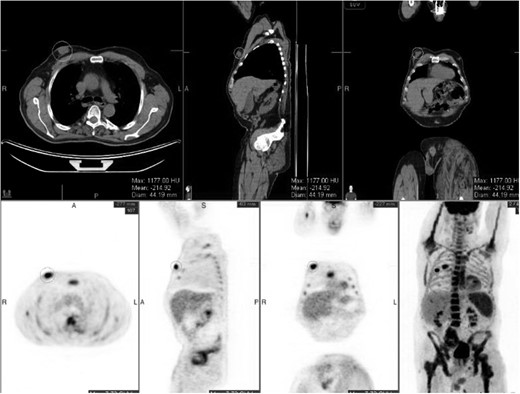
Post chemotherapy PET/CT scan. The breast mass decreased in size, with no mediastinal or hilar lymphadenopathy.
DISCUSSION
There are well-documented studies on the relationship between female breast cancer and patients with NF1, but there are only a handful of case reports on the association of NF1 and male breast cancer. Sharif et al. published one of the largest cohort studies, following 300 women with NF1 over a 30-year-period and found that women <50 years of age with NF1 had a 5-fold increase in breast cancer compared with women in the general population [5]. Furthermore, genetic studies performed by Mendes-Pereira et al. have shown that mutations in the NF1 gene in breast cancer cells afford a resistance to anti-estrogen treatments, specifically tamoxifen [6]. Walker et al. documented a 3.5-increased risk of mortality in breast cancer patients with NF1 [7]. All three of these studies suggest not only an increased risk of breast cancer in women with NF1, but a resistance to anti-estrogen treatments, and subsequently, an increased risk of death. It has been mentioned that breast cancer should be considered among the common cancer associations with NF1 and women with NF1 considered to be at moderately increased risk for the development of breast cancer.
Other genetic syndromes, such as BRCA and PTEN, that place patients at increased risk for development of breast cancer, enjoy specific screening algorithms, there are no specific breast cancer screening recommendations for women diagnosed with NF1. Digital mammography is the gold standard for screening for early stage breast cancer. However, Da Silva et al. suggest that the use of mammography is insufficient for patients with NF1, due to the high numbers of neurofibromas that many patients display and the diagnostic challenges that said nodules provide [8]. It has been suggested that patients with NF1 undergo more intensive screenings with ultrasound and magnetic resonance imaging to circumvent the presence of cutaneous lesions and to obtain a similar early detection rate compared to non-NF1 women.
Questions arise as to whether or not aggressive screening for breast cancer in NF1 individuals would provide a mortality benefit. In 2001, an analysis of US death certificates from 1983 to 1997 found that the mean age of death for NF1 individuals was 54.4 and 70.1 years in the general population [9]. This study suggests that there is a 15-year-decrease in life expectancy in neurofibromatosis type 1. A cohort study performed by Zöller et al. determined that 45–55% of NF1 individuals had a malignant neoplasm of soft tissue and connective tissue origin or a central nervous system tumor [10]. Screening for breast cancer could potentially increase life expectancy in these individuals who have been identified with NF1, but they are also susceptible to many other types of tumors, thus, further studies are needed to confirm if breast cancer screening will reduce their mortality.
We suggest early breast examination of males with NF1 followed by mammogram for any suspicious masses. In males with suspicious breast masses and a large number of neurofibromas, using ultrasound or magnetic resonance imaging can enhance detection of malignancy.
Missing the diagnosis of breast cancer in a male with NF1 can have catastrophic implications and knowledge of appropriate imaging modalities and tests as well as further elucidating the biology of these tumors through research can help us tailor neoadjuvant/adjuvant therapy for these individuals. Based on the established link between NF1 and breast cancer seen in females, it would be prudent to perform further study of NF1 males to clarify the link between NF1 and male breast cancer which will allow physicians to better serve this population.
CONFLICT OF INTEREST STATEMENT
None declared.



