-
PDF
- Split View
-
Views
-
Cite
Cite
Michela Ceriotti, Giorgia Saccomani, Francesca Lacelli, Giovanni E. Saccomani, Wide rectal duplication cyst in an adult resected by anterior approach: efficacy and recurrence, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx115, https://doi.org/10.1093/jscr/rjx115
Close - Share Icon Share
Abstract
Alimentary tract duplications are uncommon congenital abnormalities usually diagnosed and treated in childhood. Rectal involvement is extremely rare. We report the case of a 22-year-old female who presented with chronic abdominal and perianal pain; feeling of rectal fullness. Workup revealed a rectal duplication cyst. The patient underwent a complete transabdominal excision of the cyst: an hybrid laparoscopic and laparotomic technique was adopted. The hybrid isolated anterior abdominal approach is safe and feasible even for the treatment of wide rectal duplication cysts. Real recurrence in rectal duplication cysts is uncommon when the first operation was performed with radical intent.
INTRODUCTION
Alimentary tract duplications are uncommon congenital abnormalities. Isolated cystic duplications of the gastrointestinal tract are rare (1/10 000 live births). Among them, rectal involvement is extremely rare accounting for 1–8%. Most of the duplications are found in the paediatric population and involve the small bowel [1]. It has been estimated that almost 50% of developmental cysts are asymptomatic [2], being discovered during routine physical examination or ultrasonography (US). Symptoms are often related to rectal local compression: constipation, feeling of rectal fullness, lower abdominal pain, painful defecation. Symptoms may also be given by local compression of the urinary tract [3–5]. Rectal developmental cysts are commonly revealed by complications such as local infection (with a chronic perianal fistula), rectal bleeding or malignant evolution.
CASE REPORT
A 22-year-old white female was admitted to our hospital in May 2014 for chronic abdominal and perianal pain and feeling of rectal fullness.
On physical examination there were no clinical signs. On digital rectal examination a painful tender, round, smooth posterior fluctuant extraluminal mass was palpable. This finding was confirmed on sigmoidoscopy with bulging endoluminal mass with normal intestinal mucosae above the dentate line.
MRI (Magnetic Resonance Imagery) and endorectal-US revealed a wide, homogeneous, multiloculated cystic lesion (8.8 × 8.3 × 10 cm3). The mass lay on the right posterolateral pararectal space, in an extraperitoneal plan, following the course of the rectal distal portion in the context of the levator ani muscle. At IV contrast injection scans no significant contrast agent uptake by the lesion was detected (Fig. 1A–C).
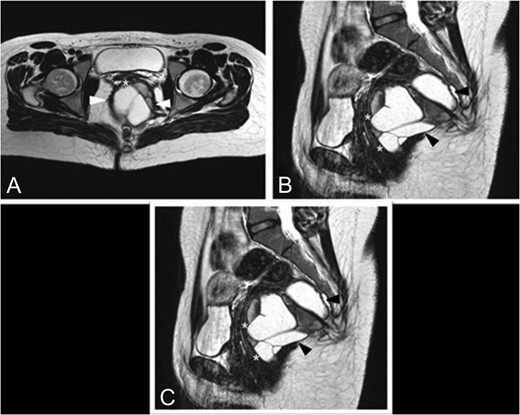
Preoperative MRI. (A) Axial TSE T2-weighted images show a large multiloculated cystic lesion (arrowhead) dislocating and closely adherent to the posterior rectal wall (*). (B) This sagittal TSE T2-weighted image shows a cystic lesion (arrowhead) expanded in the posterior pararectal space, containing serum-proteinaceous material, following the course of the rectal distal portion (*) in the context of the levator ani muscle. (C) Coronal TSE T2-weighted images demostrate the relations among the cystic lesion (black*), the rectum (white*) and the levator ani muscle (arrowhead).
A sample of the cystic fluid obtained by transvaginal biopsy revealed purulent material.
The patient underwent a complete transabdominal excision of the cyst: an hybrid laparoscopic and laparotomic technique was adopted. The identification, isolation and excision of the cyst from the rectum was performed by laparoscopy. A Pfannestiel incision was needed because of tenacious adhesions of the lower part of the cyst to the pelvic floor (coccyx). The wall of the lesion was left intact. The postoperative course was uneventful.
The pathology report described a 12 × 6 × 3 cm3 mass, containing cystic structure filled with brownish haemorrhagic fluid. Microscopic examination showed connective tissue with segments of smooth muscle covered with multi-layered squamous and columnar epithelium. This findings confirmed the diagnosis of congenital cystic rectal duplication with inflammatory characteristics.
At 8 months follow-up the patient complaint of mild constipation. On digital rectal examination a small (2–3 cm) tender fluctuant extraluminal retrorectal mass was palpable above the anal verge. At MRI the TSE T2-weighted image shows a recurrent cystic lesion expanded in the posterior pararectal space in the context of the levator ani muscle (Fig. 2A–C).
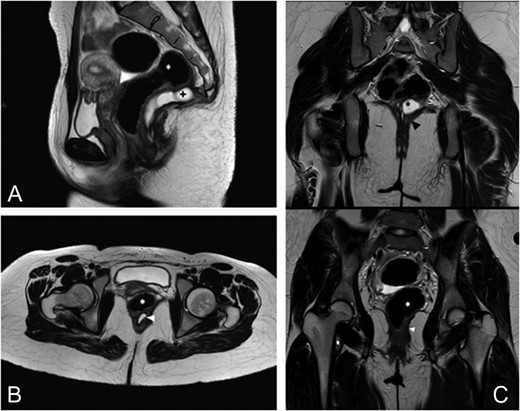
Eight months follow-up MRI. (A) This sagittal TSE T2-weighted image shows a recurrent cystic lesion (+) expanded in the posterior pararectal space, containing serum-proteinaceous material, following the course of the rectal distal portion (*) in the context of the levator ani muscle. (B) Axial TSE T2-weighted images show the cystic lesion (arrowhead) closely adhering to the posterior rectal wall. (C) Coronal TSE T2-weighted images demostrate the relations among the cystic lesion (black*), the rectum (white*) and the levator ani muscle (arrowhead).
The patient underwent a surgical excision of the recurrent duplication cyst via Karske's approach with coccygeal resection.
The pathology report described inflammatory tissue, with no evidence of recurrent intestinal cyst.
The postoperative course was uneventful, except for a wound infection that was drained.
DISCUSSION
Duplications of the alimentary tract are spherical or tubular structures which can occur anywhere in the intestinal tract. Seventy percent of all duplications are diagnosed prior to age 2 years, but they can be diagnosed at any age. Duplications are rare (1/10 000 live births) and, among them, rectal involvement is extremely rare accounting for 1–8% [6].
In view of their rare incidence, rectal duplication lesions have been misdiagnosed as haemorrhoids or fistula in ano with resultant delay in diagnosis.
Five anatomic types are described: tubular, cystic, fistulised (external or internal) and diverticular. The internal or external fistulas associated with cystic duplications may be primary or secondary to pressure, infection or ulceration and they are usually located posteriorly to the anal canal [7].
Surgical excision is curative, provides symptomatic relief and prevents complications from the cyst including sepsis and malignant degeneration.
Surgical excision of retrorectal duplication cyst is difficult because of the anatomical site and dealings: anteriorly the rectum; laterally the hypogastric plexus and its branches; posteriorly and laterally iliac vessels and the ureter; posteriorly the mean sacral artery. The major risks during this surgery is bleeding and rectal lesion.
Excision may be approached by a transanal, transcoccigeal or posterior sagittal approach [3–5, 8]. Recently also a transanal endoscopic microsurgery or a transabdominal laparoscopic approach can be used.
The last one is normally reserved to small lesions located behind the high rectum but is also particularly useful if the rectal duplication cyst has an intra-abdominal component or if it is located in the presacral space and it is large in size [9, 10].
Particularly, the isolated anterior abdominal approach has shown to be safer than the combined strategy in a series of six patients with wide benign retrorectal tumours [10]. This approach allows also the complete resection of the lesion and gives (especially to young female patients) an aesthetic advantage using Pfannestiel incision. That's the reason why we used the anterior approach in our case.
The MRI findings at 8 months follow-up have mimicked recurrent cyst, not confirmed by the pathology report. Normally, surgical excision of gastrointestinal duplication cysts is generally curative; however, follow-up is important after the treatment.
CONCLUSION
The hybrid (laparoscopic and laparotomic) isolated anterior abdominal approach provides an interesting alternative to the posterior approach with high efficacy (complete excision), low morbidity and absence of functional impairment even for wide infected cystic lesions [10].
CONFLICT OF INTEREST STATEMENT
None declare.



