-
PDF
- Split View
-
Views
-
Cite
Cite
Akiko Sakakibara, Kousuke Matsumoto, Takumi Hasegawa, Tsutomu Minamikawa, Takahide Komori, Single-stage reconstruction for buccal mucosa tumor resection including the labial commissure using a facial artery musculomucosal flap and a vermilion advancement flap, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx108, https://doi.org/10.1093/jscr/rjx108
Close - Share Icon Share
Abstract
Resection of buccal mucosa tumors may occasionally involve the labial angle and peripheral skin. Reconstruction is required when the resection involves more than one-third of the lip. We describe a single-stage reconstruction using a facial artery musculomucosal (FAMM) flap and a vermilion advancement flap after buccal mucosa resection including the labial angle. A 62-year-old woman with carcinoma in situ of the buccal mucosa underwent tumor resection. The resection included the right labial angle and peripheral skin. The resection did not lead to a massive lip defect, but a wide defect resulted on the mucosal side. The defect on the mucosal side was reconstructed using a FAMM flap, while the vermilion defect was covered using a vermilion advancement flap. Reconstruction performed using the FAMM flap and vermilion advancement flap produced aesthetically and functionally satisfactory outcomes.
INTRODUCTION
Resection of lip neoplasms may cause disturbances in labial function and/or aesthetics. Loss of labial closure affects swallowing pressure and increases the risk of misswallowing. The loss of labial closure also causes sialorrhea, which not only leads to disturbances in aesthetics, but also reduction in quality of life.
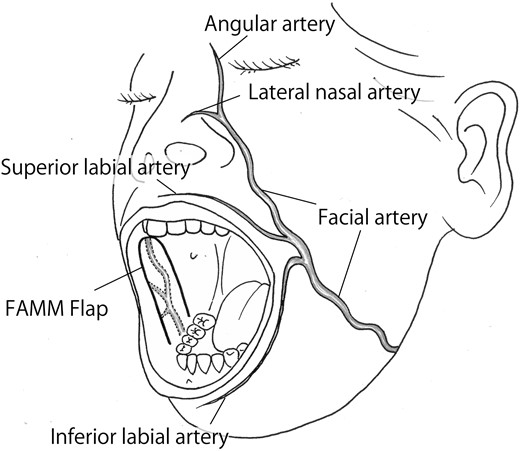
The facial artery musculomucosal (FAMM) flap includes the buccinator muscle and is pedicled by the facial artery (Fig. 1). Herein, we report a case involving the reconstruction of the labial commissure and buccal mucosa using a FAMM flap and a vermilion advancement flap that produced satisfactory outcomes.
CASE REPORT
A 62-year-old woman had a rough-surfaced tumor measuring 25 × 10 mm2 overlying the region from the mucosal surface of the right labial commissure to the lower lip (vermilion border) (Fig. 2). Positron emission tomography-computed tomography was used to detect the local invasion in the buccal mucosa (Fig. 3). A preoperative biopsy was performed, and the tumor was diagnosed as malignant (carcinoma in situ).

Intraoral photograph of the initial examination. A rough-surfaced tumor measuring 25 × 10 mm2 is visible over the region from the mucosal surface of the right labial commissure to the lower lip (vermilion border). Black sutures were used following a biopsy conducted at the previous hospital.
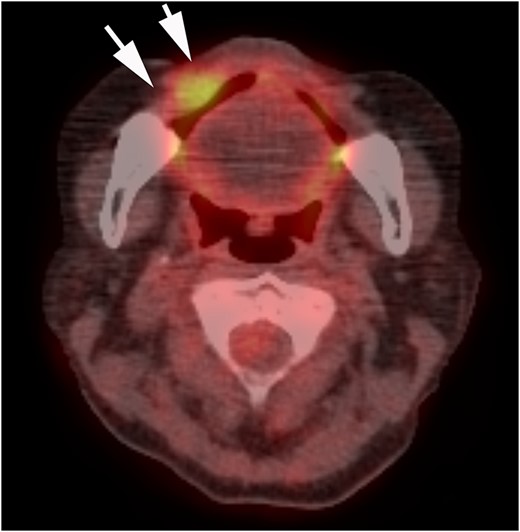
PET-CT findings. Invasion localized to the right buccal mucosa is visible (arrow).
A 10-mm safety margin was created beyond the resection line (Fig. 4a and b). The resection involved the right labial commissure and a part of the skin thickness. The extent of resection included the white upper lip and a 10-mm margin neighboring the labial commissure, as well as 5- and 10-mm widths of the upper and lower vermilions, respectively. On the mucosal side, an area ~40 × 30 mm2 in size was resected.
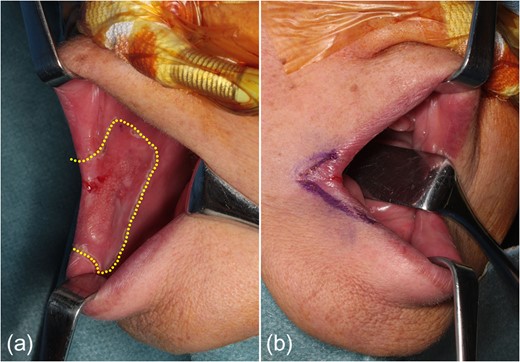
Resection range. (a) The resection measures 40 × 30 mm2 on the mucosal side. (b) The resection on the skin side includes the white upper lip with a 10-mm margin neighboring the labial commissure, and 5- and 10-mm widths of the upper and lower vermilions, respectively.
After confirmation using an ultrasonic blood flowmeter that the facial artery was not damaged, a FAMM flap was designed to involve the facial artery in the musculomucosal flap. A sufficient distance from the parotid papilla was also ensured (Fig. 5a). The musculomucosal flap measured 2 cm × 5 cm and had an inferior pedicle, wherein the central side of the facial artery was used as the base. After incision of the mucosa along the design of the flap, a further incision was made in the buccinator muscle to raise the flap, which included the facial artery deep inside the muscle (Fig. 5b). Since the resection included the modiolus, the stumps of the resected orbicularis oris muscle were sutured to establish the continuity of the muscle. The flap was rotated and sutured onto the defect in the buccal mucosa (Fig. 5c). The region from where the flap obtained was then reefed (Fig. 5d).
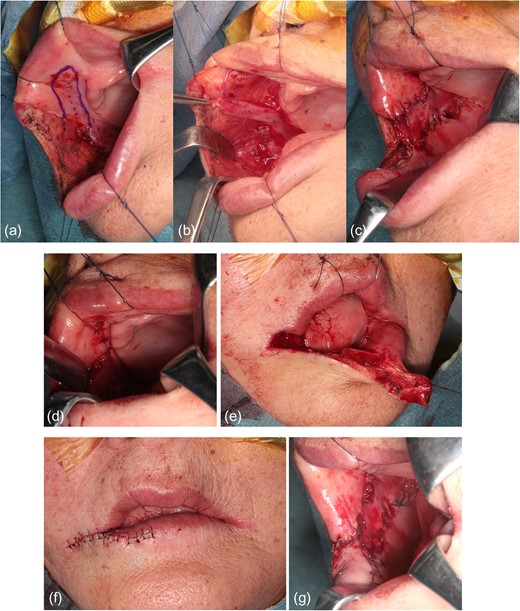
Operative findings. (a) FAMM flap design. The pedicle is close to the range of tumor resection. (b) Elevation of the FAMM flap. (c) Suture fixation of the flap in the defect of the buccal mucosa. (d) Reefing of the region from where the flap is obtained. (e) Elevation of the vermilion flap. (f) Extension of the vermilion flap followed by suture fixation in the defective area. (g) Appearance of the intraoral surface.
The lower vermilion had a larger defect than the upper vermilion. We decided to create a vermilion advancement flap from the lower lip because reefing can considerably restrict mouth opening (Fig. 5e). The lower vermilion was incised as far as the midline and extended to where it would be sutured to the upper vermilion. The mucosal side was sutured to the FAMM flap (Fig. 5f and g).
Approximately 1 year after the operation, aesthetic satisfaction was obtained and there was no restriction in mouth opening. In addition, sialorrhea was no longer present because we ensured the continuity of the orbicularis oris muscle and retention of labial closure (Fig. 6a and b).
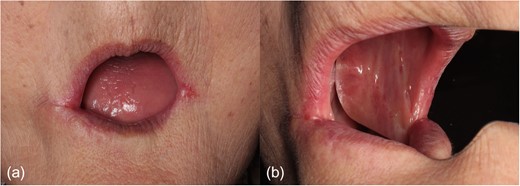
Postoperative photographs. (a) Approximately 1 year after the operation, aesthetic satisfaction is obtained. There is no restriction in mouth opening. (b) Appearance of the intraoral surface (image on the mirror).
DISCUSSION
Continuity of the orbicularis oris muscle is the basic prerequisite for securing labial closure [1]. Vermilion and buccal mucosal defects caused by tumor resection can be reefed within the limitations of functionality and aesthetics. However, simple reefing can also cause considerable restriction of mouth-opening capacity. In lip reconstruction, two impairments in particular, disturbances in functionality and aesthetics, are the indices used to evaluate outcomes [2].
Various reconstruction methods for defects have been previously used, and a various flow charts according to the range of the defect have been reported [3]. When labial commissure resection is performed, disturbances in functionality are a concern due to the likelihood of development of trismus [4]. Generally, if the range of the defect covers one-third of the lip width or more, reconstruction is required, as reported in many cases [5]. A recent technique involves the attachment of polyglycolic acid and sheet tissue adhesive to the mucosal defect, followed by secondary healing [6]. Depending on the site, functional disturbances, such as trismus, may develop [7]. This patient can use full dentures, but the attachment and detachment of this may become difficult when amount of opening decreases. However, it is important to keep continuity of the orbicularis oris muscle. If the local flap is insufficient, the orbicularis oris muscle reconstruction using a free flap, muscular fasciae and the tendon are required.
We believe that ‘reconstruction with the same tissue as the defective tissue where possible’ leads to satisfactory outcomes in terms of functionality, texture and color. Therefore, we selected the FAMM flap, which is a pedicled musculomucosal flap.
In the present case, we achieved full engraftment. It has been reported that the apical part of the musculomucosal flap undergoes necrosis even if it includes the facial artery. The reasons for this include pedicle twisting and incorrect positioning of the artery within the flap [8]. Another previous report also recommends identification of the vascular course in advance when using a FAMM flap [9].
Although the lip defect was not large, the defect in the mucosal side was wide enough to involve the muscle layer. Therefore, there was a substantial gap between the defects in the skin and those on the mucosal side. Options for the management of the vermilion defects in this case include the following: (i) simple lip reefing, (ii) transplantation of a musculomucosal flap to the lip and (iii) use of the vermilion. We considered reconstruction of the lips using the mucosa of the FAMM flap [10]. However, there was an aesthetic concern because the region where the FAMM flap, mucosal epithelium and lip were sutured together had the potential to develop a scar and an apparent asymmetry. Our goals comprised ‘securing the continuity of the orbicularis oris muscle’ and ‘reconstruction with the same tissue as the defective one where possible’. Consequently, we formed a vermilion advancement flap.
In the present case, reconstruction of a labial commissure defect due to a malignant tumor of the buccal mucosa using a FAMM flap and a vermilion advancement flap produced aesthetically and functionally satisfactory outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.



