-
PDF
- Split View
-
Views
-
Cite
Cite
Reza Ershadi, Asghar Hajipour, Mohamadrahim Vakili, Complete cricotracheal transection due to blunt neck trauma without significant symptoms, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx111, https://doi.org/10.1093/jscr/rjx111
Close - Share Icon Share
Abstract
Laryngotracheal injuries are relatively rare but their mortality rate is fairly high. Complete disruption of trachea is extremely rare and a systematic approach is needed for early diagnosis and favourable outcome. The patients symptoms and physical signs do not necessarily correlate with the severity of the injuries and this case report highlights it. This is a case report of 25-year-old man who arrived to the emergency department 8 h after a motor accident in which a rope was wrapped around his neck. Because of the good general and respiratory condition of the patient on admission, the pathognomonic signs of laryngeal injury were not noticed. A computed tomographic scan showed distortion of cricotracheal framework. Flexible bronchoscopy showed cricotracheal transaction. Immediately, the endotracheal tube was advanced distal to the transection site under bronchoscopic guide and then after neck exploration primary end-to-end cricotracheal anastomosis was performed.
INTRODUCTION
Traumatic tracheal injury after blunt neck trauma is rare; however, most patients with complete tracheal transection usually die at the accident scene due to loss of airway [1]. The few, who survive and arrive at a hospital, pose a diagnostic and therapeutic challenge to the trauma team. These patients may suffer fatal outcomes or long-term complications when misdiagnosed or treated improperly. Diagnosis is usually obscure as the symptoms may not be directed towards the disease. Early diagnosis and treatment of tracheal injuries lead to the best outcome [2]. In this article, our experience with one survivor of complete cricotracheal transection caused by blunt neck trauma, without significant symptom is reported.
CASE REPORT
A 25-year-old man arrived in the emergency room 8 h after a motor accident in which a rope was wrapped around his neck. Initial pulse oximetry saturation (SpO2) was 94%. The vital signs included a blood pressure of 122/80 mmHg, a heart rate of 98 beats/min, a respiratory rate of 23 breaths/min, and an axillary temperature of 36.2°C. Because of the good general and respiratory condition of the patient on admission, the pathognomonic signs of laryngeal injury were not noticed. Patient had skin contusion and moderate crepitus on his neck area (Fig. 1). His phonation was normal without dyspnea, cough, hemoptysis or hoarseness. Pneumomediastinum and subcutaneous emphysema were noted on a supine chest radiograph (Fig. 2). Computed tomographic (CT) scan of the neck and chest revealed pneumomediastinum, subcutaneous emphysema in the neck and distortion of laryngotracheal framework (Fig. 3). Flexible bronchoscopy showed cricotracheal transection with normal movement of true vocal cord. At the same setting, endotracheal tube was advanced distal to the transection site under bronchoscopic guide (Video). Neck exploration demonstrated complete cricotracheal separation (Fig. 4). The area was debrided and primary cricotracheal end-to-end anastomosis was performed. The patient was extubated 2 days after the surgery. Fiberoptic bronchoscopy on Days 20 and 90 showed that the tracheal injury healed completely with no apparent proliferation of granulation tissue.

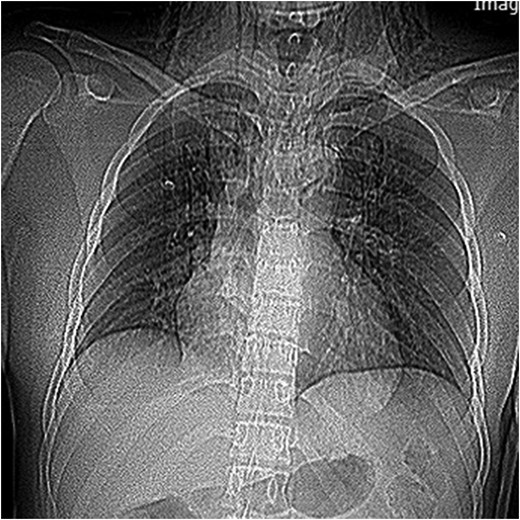
Supin chest radiograph showing pneumomediastinum and neck subcutaneous emphysema.
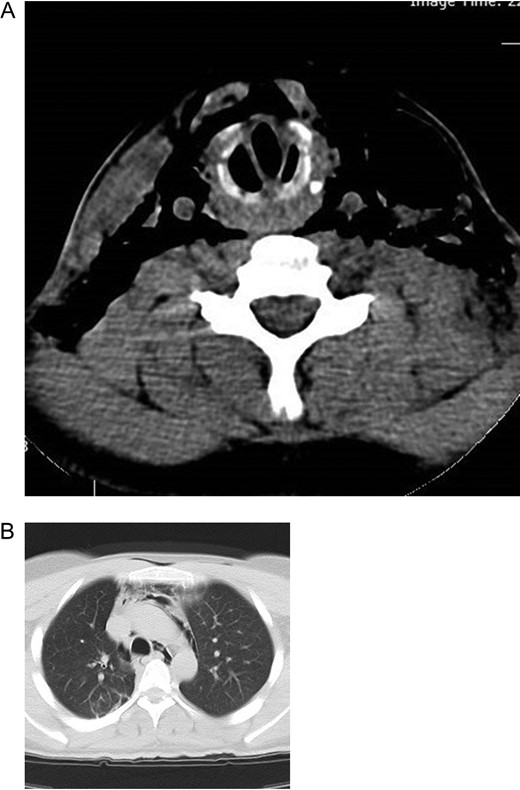
(A) CT image of the neck showing subcutaneous emphysema and larygotracheal framework distortion. (B) CT image of the chest showing pneumomediastinum.
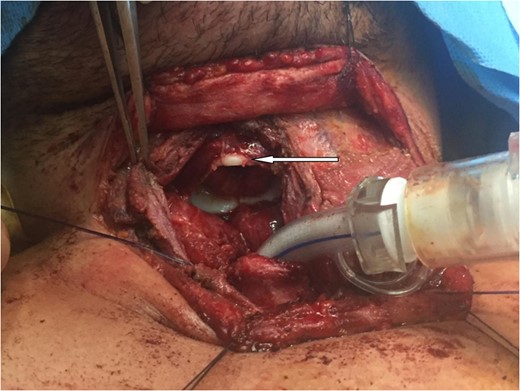
Neck exploration demonstrated complete cricotracheal separation (arrow showing cricoid).
DISCUSSION
Complete tracheal transection in blunt cervical trauma is uncommon occurrence. Laryngotracheal injuries are life threatening with mortality rate of 40%. Timely and proper airway management is life-saving [3]. Signs and symptoms may be subtle in tracheal injuries and also relatively non-specific co-relating poorly with the severity of the underlying injuries. Intact peritracheal tissue may provide a life-saving conduit for gas exchange through the disruption [4]. Most common presentations are respiratory distress, dyspnea, poor gas exchange and hemoptysis [5]. Cyanosis and serious respiratory embarrassment is present in 30% of the cases. Another common symptom is hoarseness or dysphonia, occurring in 46% of the patients [6]. The most common signs of airway injury reported in most series are subcutaneous emphysema (35–85%), pneumothorax (20–50%) and hemoptysis (14–25%); however, the lack of specificity and the occult nature of the injury frequently result in a delayed diagnosis [7]. Deep cervical emphysema and pneumomediastinum are seen in 60% of the patients with tracheobronchial injuries [6]. Many tracheobronchial injuries are not diagnosed immediately (25–68%) [5]. Physicians need to maintain a high index of suspicion related to non-specific signs such as dyspnea, cough, subcutaneous emphysema and hemoptysis [8]. The mechanism of injury, vocal changes and rapidly expanding subcutaneous emphysema in the neck are important clues [8]. Clinical examination is followed by radiologic imaging, angiography, CT and tracheo-bronchio-esophagoscopy [9]. Accurate interpretation of the chest radiograph is essential in the early diagnosis of occult upper-airway injury. A CT scan can be performed if diagnosis is uncertain on plain films [8]. Preoperative CT can be useful in assessing associated laryngeal injuries or other unsuspected chest injuries that should be dealt with at the time of surgical exploration. CT is contraindicated in hemodynamically unstable trauma patients or patients with unstable airways [6]. Helical CT with 3D reconstruction should be considered a suitable ‘screening’ test in a trauma patient suspected of tracheal rupture and may help the clinician in the decision to perform a bronchoscopy on the patient [7]. The best diagnostic investigation is bronchoscopy. Flexible bronchoscopy should be carried out first to determine the location and extent of the injury [5]. Principles of management includes prompt airway establishment, immediate exploration of the wound with appropriate investigation. Surgical repair is the treatment of choice for tracheal transection that includes complete repair of trachea with end to end anastomosis. Complete transection of the trachea should be managed by careful suturing and being cautious to avoid damage to the recurrent laryngeal nerves [10].
CONCLUSION
Complete cricotracheal transection in blunt cervical trauma is uncommon occurrence and is life threatening. Signs and symptoms may be subtle in tracheal injuries and also relatively non-specific co-relating poorly with the severity of the underlying injuries. Timely diagnosis, skillful airway management and prompt surgical repair are important for positive outcomes.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of Surgical Case Reports online.
ACKNOWLEDGEMENT
Thanks to anesthesiologist and fellowship of thoracic surgery.
CONFLICT OF INTEREST STATEMENT
None declared.



