-
PDF
- Split View
-
Views
-
Cite
Cite
Imad Elhajjar, Khalid Sayyid, Anas Mugharbil, Houssam Khodor Abtar, First reported case of paratesticular seminoma in a postpubertal cryptorchid testis, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx088, https://doi.org/10.1093/jscr/rjx088
Close - Share Icon Share
Abstract
Cryptorchidism is a very common anomaly, affecting 2–4% of male infants and is more common in premature infants. The long-term outcome despite orchidopexy still remains problematic and controversial with a risk of developing cancer 5–10 times greater than normal. Paratesticular tumors are mostly benign and very rare in children however malignant paratesticular tumors do arise, the most common being rhabdomyosarcoma. Primary paratesticular seminoma is extremely rare by itself and in most cases is associated with foci of seminoma within the testis. To the best of our knowledge, our case represents the fourth reported case of paratesticular seminoma in the published literature and being the first one in cryptorchid testis.
INTRODUCTION
Paratesticular tumors are rare; they comprise a mixed group of benign and malignant lesions and make up about 15% of all intrascrotal tumors in the older male [1]. Among the malignant tumors, the most common histotype is liposarcoma (46.4%), followed by leiomyosarcoma (20%), malignant fibrous histiocytomas (13%) and embryonal rhabdomyosarcoma (9%) [2].
Cryptorchidism, or maldescended testes, is a common clinical diagnosis in newborn boys and one of the strongest risk factors for infertility and testicular cancer [3]. About 10% of all cases of testicular germ cell tumors occur in men with a history of cryptorchidism [4]. Failure of bilateral testicular descent carries a 40-fold relative risk of malignant transformation. Seminoma still represents the most common malignancy of undescended testis, especially in intra-abdominal testis, however, germ cell tumors arising from paratesticular tissues are rare, and standardization of their treatment is not yet available [5]. We report a case of a primary paratesticular seminoma in a cryptorchid testis which is, to our knowledge, the fourth reported case of paratesticular seminoma in the published literature, and the first to be in cryptorchid testis.
CASE REPORT
This is a 39-year-old healthy male patient with history of left undescended abdominal testis that was managed at the age of 7 years by left orchiopexy. The left testis was fixed at the external ring and was planned for second stage orchiopexy, but the patient was lost to follow up. At 39 years of age, the patient presented with localized severe left hemiscrotal and inguinal pain of one day duration. Physical examination demonstrated a fixed testis at the left external inguinal ring with marked hardness of the surrounding paratesticular tissue. A brief course of oral antibiotics for suspected left epididymo-orchitis failed to improve his symptoms. Laboratory tests showed ß-HCG: <1.2 mIU/ml (reference range: 0–4 mIU/ml); alfa-fetoprotein: 1.39 ng/ml (reference range: ≤7 ng/ml); and LDH: 247 U/l (reference range: 135–225 U/l). Testicular ultrasound revealed a small left testis of heterogeneous echotexture and measuring 2.8 × 1.7 cm2 and it contained multifocal calcifications (Fig. 1). It was located high in the scrotal sac at the end of the inguinal canal. There was inflammation and swelling of the left spermatic cord.
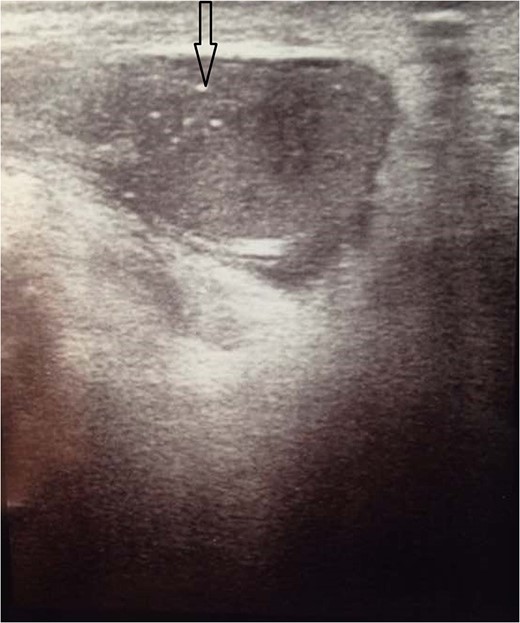
Ultrasound of the testicles showed very small atrophic left testis measuring about 2.8 × 1.7 cm2 with multiple calcifications within it (black arrow).
Left radical orchiectomy was done through left inguinal incision. Macroscopically, the testis was found to be atrophic with surrounding hard tissue. Pathologic examination revealed atrophic testicular parenchyma with hyalinized tubules and total absence of germ cells (Fig. 2). Focal interstitial chronic inflammatory infiltrates were noted. Fragments from the tissues surrounding the testis (but separate from it) showed neoplastic cell proliferation arranged in nodules of variable size, separated by fibrous bands and composed of large polyhedral tumor cells having large centrally located nuclei, prominent nucleoli and clear cell delimited cytoplasm (Fig. 3). The pattern was consistent with classic seminoma. Postoperative staging CT scan of chest, abdomen and pelvis demonstrated no abnormalities.
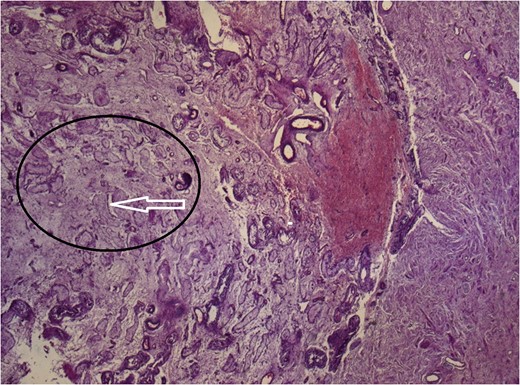
Atrophic testicular parenchyma (black circle) with hyalinized tubules (white arrow).
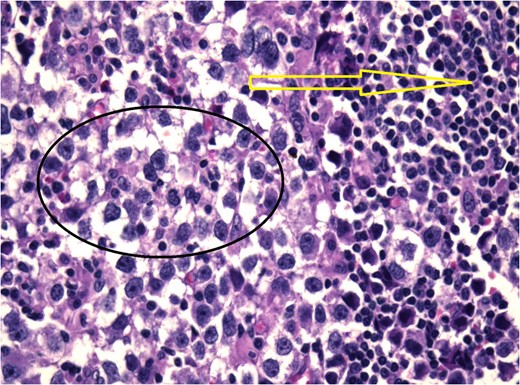
Histological examination showed nodules that contain neoplastic cell (black circle) with lymphocytic infiltration (yellow arrow).
DISCUSSION
Approximately 75% of paratesticular tumors are benign with malignant tumors accounting for 20–25%. Primary paratesticular seminoma is extremely rare [6]. This is to our knowledge only the fourth case report of a true primary paratesticular seminoma.
The association between cryptorchidism and testicular germ cell tumor has been well documented since the 1940s. Cryptorchidism is an accepted risk factor with a relative risk of 3.7–7.5 times higher than the scrotal testis population [7]. Although cryptorchidism is a risk factor for testicular seminoma, there is no published case of paratesticular seminoma associated with cryptorchidism. Among paratesticular tumors, the most frequently reported benign tumors are hemangiomas, lymphangiomas, leiomyomas and lipomas [8].
Dutkiewicz et al. [9] described a case report of a paratesticular seminoma; however, there were micro-foci of seminoma in the testis in this case and it was felt to be a burnt out primary seminoma of the testis. Early reports of epididymal seminoma are found in the literature [10], but on closer scrutiny these were all associated with foci of seminoma within the testis and were considered to arise from the testis rather than originate from the epididymis itself [6]. Dowling et al. [6] reported a case of patient who underwent a scrotal ultrasound, which suggested a simple epididymal adenoma, which after histological examination was found to be a primary epididymal seminoma.
In our patient, cryptorchid testis was found to be atrophic and showed absence of malignancy, and the epididymis showed no malignant cells. Seminoma was only detected in the tissues surrounding the testis.
Primary paratesticular seminoma in the absence of seminoma within the testis is extremely rare. The described case represents, to the best of our knowledge, the fourth reported case in the literature, and the first case reported for cryptorchid testis. The patient received single dose of adjuvant chemotherapy consisting of carboplatin (AUC 7).
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest, financial or otherwise, related to the publication of this study or its findings.



