-
PDF
- Split View
-
Views
-
Cite
Cite
Rocco Severino, Paolo Severino, Fronto-orbital mucocele with intracranial extension: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx107, https://doi.org/10.1093/jscr/rjx107
Close - Share Icon Share
Abstract
Frontal sinus mucoceles are benign, pseudocystic lesion deriving from the obliteration of the sinus ostium, resulting in a continuous mucous accumulation. The growing process of a mucocele leads to a progressive enlargement of the sinus cavity, thickening and eroding its bony walls up to invading the surrounding tissues. The surgical procedure through an endoscopic endonasal approach is the current treatment option for such conditions, but in cases with an extensive bone erosion and intracranial or intraorbital extension, a transcranial approach should be preferred. We report a case of a frontal sinus mucocele with unusual intraorbital and intracranial extension, causing exophthalmos and ophthalmoplegia, removed through a transcranial frontal approach and the subsequent obliteration of the sinus.
INTRODUCTION
Mucoceles are benign, pseudocystic, mucous-secretory lesions. Their expansion is due to a continuous mucous secretion, with progressive enlargement of the mass that causes displacement of the surrounding tissues and erosion of the bony walls of the sinus cavity.
Mucoceles derive from the obliteration of sinus ostium, that can be whether congenital or acquired (allergic rhinitis, post-traumatic, post-inflammatory, infective) [1].
Frontal sinuses are the most commonly involved by mucoceles, whereas ethmoidal air cells come after [2]. Common symptoms are headache, exophthalmos, ptosis and diplopia; if an erosion of the posterior wall of the sinus has occurred, with consequent invasion of the anterior cranial fossa, the contaminated content of the mucocele may cause a meningitis or a brain abscess with or without a CSF fistula.
The radiological diagnosis and the pre-operative surgical planning are based on CT scan, that shows the extension of the bone erosion, and on the MRi that is useful for the evaluation of the soft tissues displacement. The surgical procedure consists in the total removal of the mucocele and its contents, followed by the obliteration of the sinus. We report a case of a 65-year-old woman with a recent history of ptosis and ophthalmoplegia, due to a frontal sinus mucocele causing bone erosion with extension in the cranial and the orbital spaces.
CASE REPORT
A 65-year-old female attended to our observation describing a 4-week history of left exophthalmos, which had worsened in the previous days with the association of ptosis, ophthalmoplegia and diplopia. She had no history of head trauma or previous naso-sinusal surgery. A MRI and a CT of the skull revealed a hyperintense lesion on T2-weighted images occupying the left frontal sinus that partially eroded the orbital roof and the frontal posterior wall of the sinus, with invasion of the left orbit and displacement of the ocular globe and intracranial extension without dural infiltration (Fig. 1).
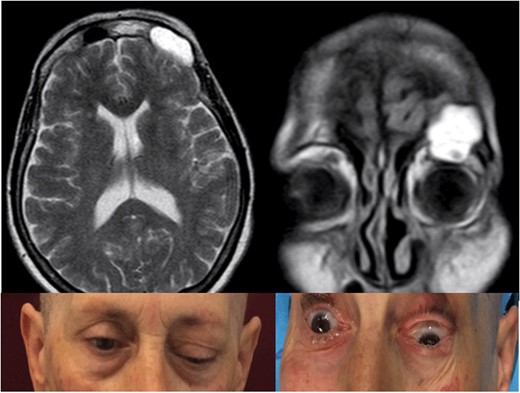
Pre-operative T2-weighted MRi showing a frontal sinus mucocele with intraorbital and intracranial extension, causing ptosis, exophtalmus and diplopia.
We performed a left coronal skin incision and a frontal craniotomy in order to obtain a wider explosion of the lesion and to obliterate the sinus cavity easier. The mucocele was removed through aspiration of its mucosal part and microsurgical dissection of its capsule from the external dural layer of the frontal pole and the superior surface of the periorbita. Successively, after the removal the remaining posterior sinus wall and all the residual sinus mucosa, we obliterated the surgical cavity with abdominal fat covered with pericranial flap and replaced the original bone flap to close the craniotomy (Fig. 2A–C).
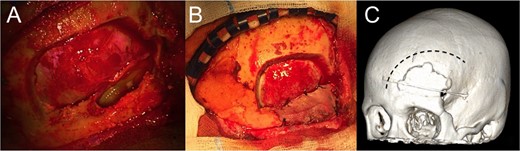
(A) left frontal craniotomy and aspiration of the mucocele, demonstrating a wide communication between the intracranial and the sinusal spaces; (B) the surgical cavity, emptied of the mucocele, has been filled with abdominal fat and closed with pericranium and dural patch; and (C) 3D rendering of the approach.
In the post-operative period the patient underwent a standard antibiotic prophylaxis (ceftriaxone 1 g × 2/die IV) for the successive 4 days and was discharged after 5 days with no neurological or systemic complication. The histological examination confirmed the intraoperative diagnosis of mucocele, and 1 month after the procedure, the patient showed a good improvement of the exophthalmos and ophthalmoplegia with a radiological evidence of complete sinus obliteration (Fig. 3).
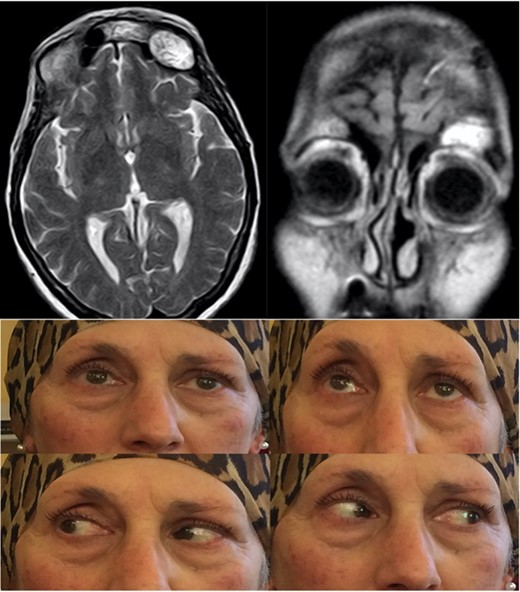
Post-operative T2-weighted MRi showing the fat tissue filling the surgical cavity, with improvement of the ptosis and absence of diplopia.
DISCUSSION
An occlusion of a sinus ostium, caused by congenital malformation or infective, inflammatory or tumoral process leads to a progressive accumulation of the sinus mucosa secretions, with the development of a mucocele. These pseudocystic lesions are characterized by a gradual expansion through a continuous mucous-secreting process, resulting in a compression and displacement of the surrounding soft tissues and erosion of the bone walls, due to a dynamic process of bone resorption and formation [3].
Mucoceles are commonly located in the frontal sinus, whereas the ethmoidal air cells, the sphenoidal and maxillary sinuses come after.
The most common sign of a frontal sinus mucocele is a bifrontal headache; if an orbital invasion has occurred the patient usually develops a visible mass in the orbital upper quadrants with proptosis, with or without disturbances of ocular motility and epiphora. If the mucocele has an intracranial extension, it can erode both the posterior and the anterior wall of the sinus; the posterior wall is usually thinner than the anterior one, and its erosion may cause several and potentially dangerous complications, such as an epidural abscess, a subdural empyema a CSF leak or a meningitis, while the less frequent erosion of the anterior wall appears as a fluctuant swelling under the skin of the eyebrow and of the forehead.
The radiological assessment is based on the CT scan, even thought a plain skull radiography showing enlarged sinus walls and signs of bone erosion can be suspicious of a mucocele. However, CT is the most useful investigation in identifying a mucocele, that appears as an airless mass inside the sinus, non-enhancing and with mucous density [4], and its relations with the orbital walls, the ocular globe and the anterior cranial fossa, in addition to signs of bone erosion.
The MRI is helpful in defining the mucous component of the mass but the intensity on T1 and T2-weighted images is not univocal, depending on the grade of hydration and viscosity of the mucocele; besides, post-contrast sequences differentiate a mucocele, usually not showing contrast enhancement, from other naso-sinusal tumors.
The management of mucoceles is based on the surgical excision of the mass. In the case reported we performed, as suggested by many authors [5], a transcranial approach that allowed a wide exposition of the frontal sinus, a safer removal of the mucocele and an easier obliteration of the sinus using both subcutaneous abdominal fat and pericranial flap in order to isolate the surgical cavity from the intracranial space and minimize the risk of post-operative infections. The alternative endoscopic trans-sinusal approach is not recommended in such cases because of the intracranial extension of the mass [6, 7], with higher risk of intracavitary residual and post-operative recurrences due to a narrow access to the lesion [8]. The surgical management through a transcranial frontal approach and successive sinus obliteration is, in our opinion and after a literature analysis, the best treatment option in cases of mucoceles with both intracranial and intraorbital extension.
The prognosis is usually favorable but, although a low recurrence rate, a long follow up is generally recommended [9, 10].
CONFLICT OF INTEREST STATEMENT
None declared.



