-
PDF
- Split View
-
Views
-
Cite
Cite
Katsunori Asai, Hajime Nakamura, Takeo Nishida, Shayne Morris, Takayuki Sakaki, Overlapping stent-assisted coil embolization for a ruptured intracranial vertebral artery dissection, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx105, https://doi.org/10.1093/jscr/rjx105
Close - Share Icon Share
Abstract
Ruptured intracranial vertebral artery dissection is a cause of non-traumatic subarachnoid hemorrhage. Urgent intervention should be considered to prevent fatal rebleeding. Endovascular parent artery occlusion, which is the initial treatment of choice, is not suitable for patients with a hypoplastic or occlusive contralateral vertebral artery. We report a case of ruptured vertebral artery dissection, which was successfully treated with double overlapping stent-assisted coiling.
INTRODUCTION
Ruptured intracranial vertebral artery dissection (VAD) is one of the causes of non-traumatic subarachnoid hemorrhage (SAH) [1–4]. Because rebleeding from VAD may occur at an early stage [1], urgent intervention will be considered [2]. Endovascular parent artery occlusion (PAO) is the initial treatment of choice for VAD [2, 3]. However, PAO is not suitable for patients with VAD and a hypoplastic or occlusive contralateral vertebral artery [2, 5]. Moreover, PAO has a risk of postoperative medullary infarction, which results from occlusion of perforators branching from the vertebral artery [3]. With recent improvement of intracranial stents, reconstructive therapies are increasingly emerging [4–6]. Multiple overlapping stent-assisted coiling is an adjunctive technique in treatment of complex cerebral aneurysms [7]. We report a case of ruptured VAD, which was successfully treated with double overlapping stent-assisted coiling.
CASE REPORT
A 48-year-old man was admitted to our hospital because of loss of consciousness after a sudden nuchal pain. Brain computed tomography (CT) showed diffuse SAH (Fig. 1A). The following CT angiogram showed a fusiform aneurysm at the right vertebral artery with contralateral hypoplasia (Fig. 1B). The endovascular procedure was performed under general anesthesia. The patient received a loading dose of 200 mg of aspirin and 300 mg of clopidogrel via a nasogastric tube. A preoperative angiogram showed VAD with a blister at the pseudolumen (Fig. 2A). Initially, a stent (Enterprise, 4.5 mm × 37 mm; Codman, Raynham, MA, USA) was deployed from the basilar artery to the right vertebral artery. A second stent (Enterprise2, 4.0 mm × 30 mm) then overlapped the first stent, covering the pseudolumen (Fig. 2B). Coiling was performed from a microcatheter (Excelsior SL-10/45; Boston Scientific, Fremont, CA, USA), which was jailed in the pseudolumen. After the first coil perforated the blister, a balloon catheter (Scepter C, 4.0 mm × 15 mm; Microvention, Tustin, CA, USA), which was exchanged with a stent delivery catheter, was inflated in the stent. All five small platinum coils (Target nano, 2 mm × 4 cm and 1.5 mm × 2 cm; Stryker, Fremont, CA, USA) completely occluded the pseudolumen (Fig. 2C), and the right vertebral artery was preserved (Fig. 2D). Magnetic resonance imaging, which was obtained 3 weeks after the procedure, showed right cerebellar infarction without damage of the brainstem (Fig. 3). The patient recovered and returned to his former job after 2 weeks of intensive care and 3 months of rehabilitation therapy. An angiogram, which was obtained 6 months after procedure, showed no recurrence of VAD (Fig. 4).
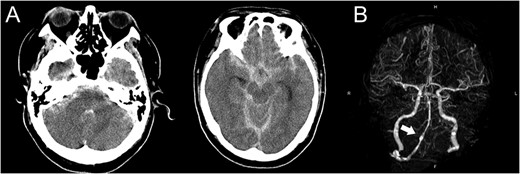
(A) Computed tomography images show diffuse subarachnoid hemorrhage. (B) Computed tomography angiogram shows a fusiform aneurysm at the right vertebral artery (arrow) with contralateral hypoplasia.
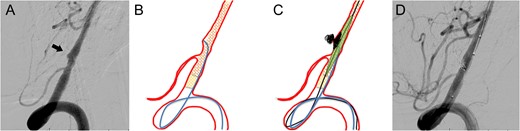
(A) Preoperative angiogram shows a dissecting aneurysm with a blister. (B) The first stent was deployed across the aneurysm and the second stent overlapped the first stent. (C) Coiling was performed under the support of a balloon catheter after the first coil perforated the blister. (D) Complete obliteration of the pseudolumen was achieved and the parent artery was preserved.
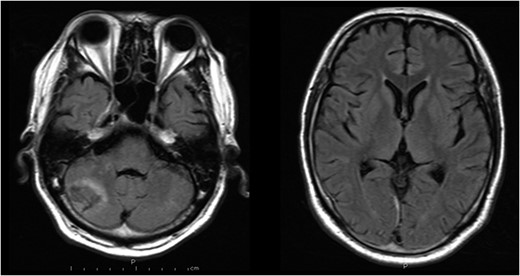
Magnetic resonance images obtained 3 weeks after the procedure shows right cerebellar infarction without damage of the brainstem.

Angiogram obtained 6 months after the procedure shows no recurrence of vertebral artery dissection.
DISCUSSION
The concept of stent therapy for VAD is to crimp the intimal flap to the vessel wall and obstruct the pseudolumen [8]. A meta-analysis showed that reconstructive therapy (including stenting alone, stent-assisted coil embolization and flow diverter stenting) was not inferior to deconstructive therapy (including PAO and trapping) for a favorable neurological outcome [9]. However, reconstructive therapy has a risk of angiographic recurrence. Single stent-assisted coiling has a higher recurrent rate than multiple overlapping stent-assisted coiling for patients with a ruptured VAD [5]. One of the reasons was considered that a stent-related favorable hemodynamic change was achieved in the latter technique. In stent-assisted coiling, placement of small coils <3 mm has a risk of coil migration through the stent strut [10]. The overlapping stent, which reduced the stent strut porosity, could avoid the escape of small coils in this case.
In conclusion, in patients with ruptured VAD with contralateral hypoplasia, as in our case, overlapping stent-assisted coil embolization might be effective for preventing rebleeding and angiographic recurrence.
CONFLICT OF INTEREST STATEMENT
None declared.



