-
PDF
- Split View
-
Views
-
Cite
Cite
Chung-ching Lee, Wing-kei Choi, Jimmy Yu-wai Chan, Candida parapsilosis associated with cervical necrotizing fasciitis and descending mediastinitis, Journal of Surgical Case Reports, Volume 2017, Issue 4, April 2017, rjx065, https://doi.org/10.1093/jscr/rjx065
Close - Share Icon Share
Abstract
This report presents an immunocompetent lady suffering from Candida parapsilosis associated with polybacterial cervical necrotizing fasciitis and descending mediastinitis. A literature review and management of invasive candidiasis is discussed.
A 57-year-old healthy lady presented with cervical necrotizing fasciitis and descending mediastinitis. She was promptly managed with emergency debridement. Both blood and tissue culture yielded multiple microorganisms including C. parapsilosis.
The patient recovered progressively. She was discharged 2 months later.
Fungal infection is emerging in this medical era. Vigilance in patient management and as well as considering atypical microorganisms in aetiology may improve patient outcome.
INTRODUCTION
Cervical necrotizing fasciitis is a serious and potentially life threatening head and neck infection. When it is complicated with descending mediastinitis and septic shock, the mortality can be doubled, up to 41% [1].
We would like to describe a patient who suffered from synergistic fungal and polybacterial cervical necrotizing fasciitis with descending mediastinitis, complicated with empyema thoracis. To our understanding, there has been no previous literature reporting Candida parapsilosis associated with cervical necrotizing fasciitis and descending mediastinitis.
CASE REPORT
A 57-year-old lady, a non-smoker and non-drinker with good past health, presented with a week’s history of sore throat, runny nose and productive cough. Upon admission, she was having high fever and sinus tachycardia. Her neck had skin erythema and crepitus on palpation. Oxygen saturation was maintained. Her lateral neck radiograph showed the presence of retropharyngeal gas and chest radiograph noted consolidative changes at the right lower zone. A septic work-up was performed and her laboratory evaluation revealed significant metabolic acidosis.
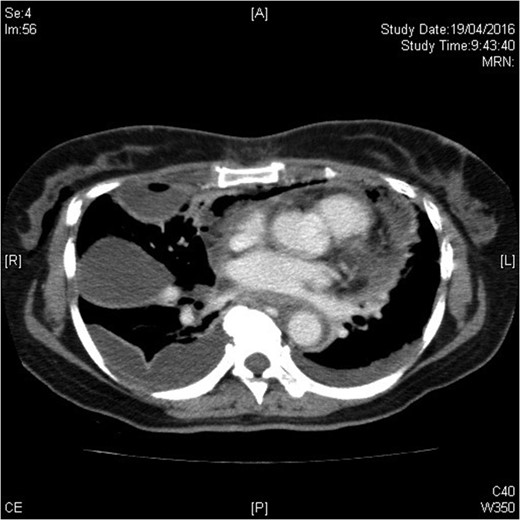
The urgent contrast computed tomography neck and thorax revealed multiple gas locules in bilateral deep cervical spaces, loculated right pleural effusion and right chest wall subcutaneous emphysema. The overall radiological features were suggestive of underlying deep neck space infection by gas-forming organisms complicated with descending mediastinitis and empyema thoracis (see Figs 1–3).
Emergency surgical debridement and drainage were performed by combined bilateral transcervicotomy and right video-assisted thoracoscopic approaches. All deep neck spaces down to mediastinum were opened. A moderate amount of turbid fluid was drained and necrotic fascia and muscle were debrided. The remaining collection inside the thoracic cavity was drained through thoracoscopic approach. The neck wound was laid open and packed with gauze. Multiple right lower posterior teeth with severe periodontitis were extracted. Chest drains were inserted at the conclusion of operation.
The patient required high dose inotropes throughout the operation. She was kept intubated in ICU afterwards. Daily wound examination and dressing was done. Second look wound exploration and debridement were performed on Day 3. Residual collection over the superior mediastinum and right parapharyngeal space was drained. The patient was tracheostomised. A feeding tube was inserted to help build up her nutrition. She was dependent on inotropic and ventilatory supports during the first 4 weeks. Her neck wound was amenable to primary closure 6 weeks after the first debridement. The tracheostomy was successfully decanalised. She was provided with a course of swallowing rehabilitation and was discharged 2 months later.
Histopathology sectioning of the right carotid sheath, fascia and mediastinal tissue confirmed necrotizing inflammation. Both blood and deep neck tissue cultures recovered C. parapsilosis. The carotid sheath tissue and pleural fluid recovered Peptostreptococcus micros, Bacteroides pyogenes and Prevotella buccae. Intravenous anidulafungin was added to her existing broad-spectrum antibiotics.
DISCUSSION
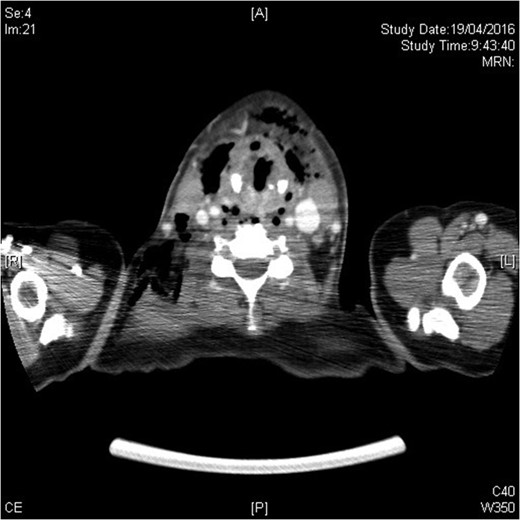
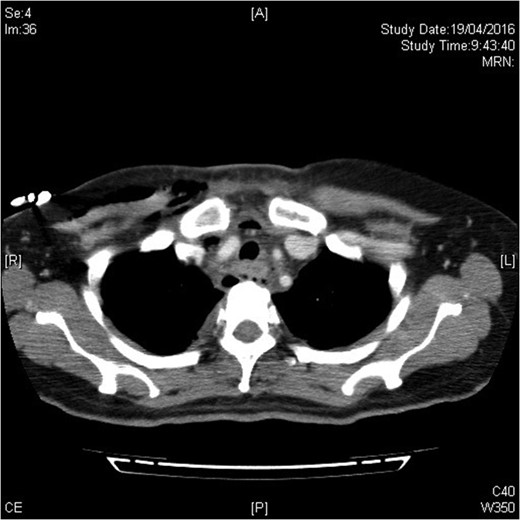
Infection extending down to superior mediastinum and chest wall.
Fungal infection in cervical necrotizing fasciitis is exceedingly rare. Reported cases usually involved immunocompromised individuals such as uncontrolled diabetics. They suffered from polybacterial and invasive fungal infections, and most if not all had fatal outcomes. Candida albicans was once reported to be the sole organism on a diabetic patient having Fournier’s gangrene [3]. Non-albicans Candida is believed to be less pathognomic. However, there is an increasing incidence of non-albicans infection and can be associated with a mortality rate of up to ~45% [4]. Candida parapsilosis is one of the five common Candida species encountered in clinical practice and those five species account for 90% of all cases of invasive candidiasis. Candida parapsilosis predominantly affects preterm neonates, especially those with indwelling catheters. The mortality rate is up to 10% [5].
Candidaemia is by far the most frequent clinical syndrome of invasive candidiasis. It can be associated with deep tissue infection, such as intra-abdominal candidiasis, candida endocarditis, ocular candidiasis and candida meningitis. The gold standard for diagnosis of invasive candidiasis is tissue or blood culture. However, the sensitivity of picking up deep tissue infection using culture based tests alone is low. Various non-culture based diagnostic tests, namely the 1-3-beta-d-glucan (BDG), the mannan Ag/anti-mannan Ab assay, and polymerase chain reaction (PCR) are employed to enhance the sensitivity to diagnose invasive candidiasis and they may have the potential to identify patients with deep-seated candidiasis missed by blood cultures in clinical practice [6].
Candida parapsilosis is known for its ability to form biofilms and has a higher minimal inhibitory concentration (MIC) to echinocandins when compared with other Candida species. In the laboratory, the higher MIC is evidenced by its naturally occurring polymorphism at the hotspot Region 1 of the FKS1 gene [7]. Hence, in the past, fluconazole and other azoles were the preferred agents over echinocandins. However, the empirical use of echinocandins has not been translated into clinical failure and is not necessarily leading to worse outcomes as found by a Spanish study [8]. According to the recommendations in Infectious Diseases Society of America 2016 guidelines, they suggest using echinocandins as the initial therapy for non-neutropenic patients with candidemia, while fluconazole still remains as a valuable alternative and a step-down medication [9].
CONCLUSION
We have described an immunocompetent lady who suffered from polybacterial cervical necrotizing fasciitis with descending mediastinitis and empyema thoracis complicated by C. parapsilosis. The source of infection was likely from the oral cavity, as evidenced by the presence of poor dentition and various tissue and blood culture results. This patient demonstrated the emerging importance of complicated fungal infections. We suggest sending tissue samples not only for bacterial cultures but also fungal cultures routinely. The use of non-culture based assays for recovering fungal infection may be useful for early diagnosis and hence treatment, but this is dependent on the availability of hospital resources.
FINANCIAL DISCLOSURE
None.
CONFLICT OF INTEREST STATEMENT
None declared.



