-
PDF
- Split View
-
Views
-
Cite
Cite
Byung Seo Choi, Geon Young Byun, Seong Bae Hwang, Bum Hwan Koo, Sung Ryul Lee, Long-segment hypoplasia of great saphenous vein with posterior accessory saphenous vein as a connecting vein: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx058, https://doi.org/10.1093/jscr/rjx058
Close - Share Icon Share
Abstract
Aplasia or hypoplasia of great saphenous vein (GSV) is relatively common. Most of them are segmental and localized around the knee. They rarely extend to the inguinal area, yet in case of this, the anterior accessory saphenous vein (AASV) is the most common connecting vein. We report a case of a 22-year-old male who underwent surgery for pain and heaviness of the right calf. He had the hypoplasia of right GSV extended from below the popliteal crease to near the saphenofemoral junction with posterior ASV (PASV) as a connecting vein. Significant reflux was observed in PASV and GSV which are proximal to PASV. High ligation and stripping was performed, and symptoms improved after surgery. In this report, the author discussed a rare case of long-segment hypoplasia of GSV with PASV as a connecting vein.
INTRODUCTION
In general, the great saphenous vein (GSV) starts with medial marginal vein at the ankle, passes through saphenous compartment, and ends at the saphenofemoral junction (SFJ) [1]. The vein running out of the saphenous compartment is classified as accessory vein or tributary vein [2]. Usually, the diameter of GSV increases from feet to the groin area [2]. If the diameter of the GSV becomes smaller or diminished, it is called as GSV hypoplasia or aplasia [1, 3]. Most of them is a segmental condition localized to a part of the GSV and has vein that connect the start and end points of the hypoplastic or aplastic segment [3]. This connecting vein usually travels outside the saphenous compartment. However, there were reports of hypoplasia extended up to the groin rather than a segmental condition located around the knee. Even in these cases, most of them has anterior accessory saphenous vein (AASV) as a connecting vein [3, 4]. The purpose of this study is to report a case of long-segment hypoplasia of GSV with posterior ASV (PASV) as a connecting vein.
CASE REPORT

Photograph of posterior accessory saphenous vein (arrow) and its tributary (arrow head).
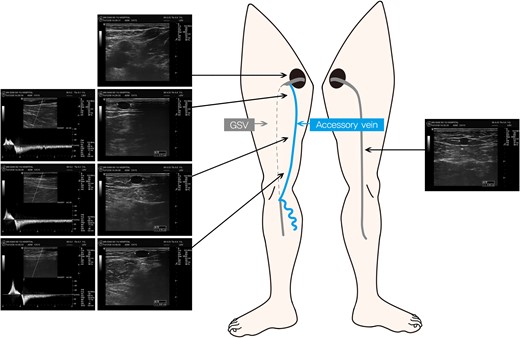
Schema of the right limb veins and findings of duplex ultrasonography. Dotted gray line represents the hypoplastic segment of the GSV and solid blue line represents the posterior accessory saphenous vein.
DISCUSSION
Aplasia or hypoplasia of GSV is known to be found in about 12~39.9% of general population and they are unilateral in general [2, 3, 7]. According to reports, aplasia or hypoplasia of GSV is more commonly observed in patient with varicose vein than without varicose vein [1, 2]. While these are common conditions, the etiology is not clearly identified. The reason for more frequent reflux in these patients is thought to be because the connecting vein (accessory saphenous vein) has thin wall and poor muscle composition compared to GSV [7], and it's surrounded solely by subcutaneous fat without supporting structures such as saphenous fascia of GSV which can prevent vasodilation [3].
Since normal GSV is located inside the saphenous compartment, it is easily detected using ultrasonography. Likewise, aplasia, hypoplasia or connecting veins can be detected using ultrasonography. Most of these connecting veins are located adjacent to the skin [2]. Endothermal ablation which is the standard treatment for varicose vein [8] has a risk of thermal injury to the skin and cannot be easily performed for connecting vein [2]. In our case, we used high ligation and inversion stripping instead of endothermal ablation to prevent thermal injury of the skin.
Aplasia or hypoplasia of GSV is uncommon at proximal or distal GSV, and usually segmental around the knee [2, 3]. In most cases, aplasia or hypoplasia starts from the upper calf to the lower thigh (92.8%). However, a few cases of hypoplasia continuing to inguinal region (2.4%) with AASV as connecting vein are reported [2]. But the AASV is known to be located slightly lateral to the GSV and aligned with femoral vessel [9]. In our case, long-segment hypoplasia of GSV was detoured from the lower part of popliteal crease to groin through PASV which is located medial to the GSV and femoral vessel, and this case is rarely reported.
There are large variations in forms and range of hypoplasia or aplasia of GSV. Therefore accurate preoperative ultrasound examination of the anatomy of the GSV and its tributaries is necessary. In this report, the author discussed a rare case of long-segment hypoplasia of GSV with PASV as a connecting vein.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
FUNDING
The authors have no sources of funding to declare.
ETHICAL APPROVAL
This study received approval from IRB at KoNIBP.
INFORMED CONSENT
The authors confirmed that written informed consent was obtained from the patient for publication of this case report and accompanying images.
REFERENCES
Author notes
First author: Byung Seo Choi, M.D.



