-
PDF
- Split View
-
Views
-
Cite
Cite
Alexandra M. Limmer, Zackariah Clement, Extensive small bowel intramural haematoma secondary to warfarin, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx044, https://doi.org/10.1093/jscr/rjx044
Close - Share Icon Share
Abstract
Intramural haematoma is a rare complication of oral anticoagulant therapy, occurring in 1 in 2500 patients treated with warfarin. This report describes a 71-year-old gentleman who presented with tachycardia, vomiting and abdominal distension on a background of anticoagulation for a metallic aortic valve. He was found to have a supratherapeutic international normalized ratio (INR) of 9.9 with an extensive small bowel intramural haematoma and secondary small bowel obstruction. He was successfully managed non-operatively with fluid resuscitation, INR reversal, bowel rest and nasogastric decompression. The patient's presentation was atypical with a lack of classic symptoms such as abdominal pain. This highlights the importance of considering intramural haematoma as a differential diagnosis for gastrointestinal symptoms in anticoagulated patients.
INTRODUCTION
Intramural haematoma is a rare complication of oral anticoagulant therapy, occurring in 1 in 2500 patients treated with warfarin [1]. The majority of intramural haematomas are small and can be managed non-operatively [2]. The following case demonstrates an extensive warfarin-related small bowel intramural haematoma with secondary bowel obstruction that was effectively managed non-operatively.
CASE REPORT
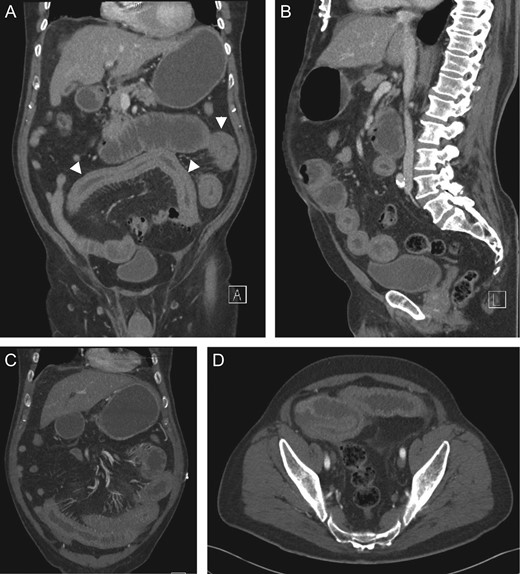
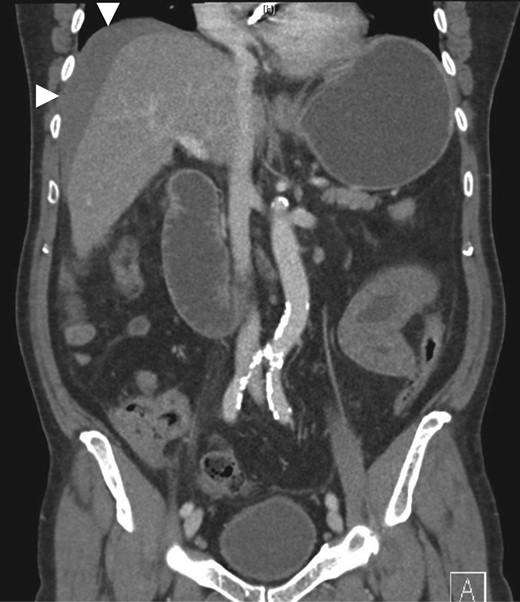
Coronal (A, C), sagittal (B) and axial (D) CT showing small bowel intramural haematoma up to the mid-ileum with associated oedema causing obstruction and proximal small bowel and gastric dilatation.
DISCUSSION
Intestinal intramural haematoma is characterized by separation of the intestinal wall layers due to slow haemorrhage from terminal arteries in the submucosa. It is a rare cause of small bowel obstruction [2, 3]. Over 90% of cases occur secondary to blunt abdominal trauma [2]. The leading cause of non-traumatic ‘spontaneous’ intramural haematoma is supratherapeutic anticoagulation with warfarin [3]. Risk factors associated with gastrointestinal bleeding on warfarin include previous gastrointestinal bleed, advanced age, comorbidities (including atrial fibrillation, renal insufficiency and chronic liver disease) and co-administration with antiplatelet agents or medications that compete for metabolism by CYP3A4 enzymes (such as fenofibrate, as seen in this case) [4, 5]. Although NOACs (rivaroxaban, apixaban and dabigatran) have reduced risk of intracranial haemorrhage, major bleeding into any site and all-cause mortality compared to warfarin, they are associated with increased risk of major gastrointestinal bleeding (RR1.25) due to their intraluminal anticoagulant activity [4, 6].
Other predisposing factors for spontaneous intramural haematoma include coagulopathies (e.g. haemophilia, von Willebrand's disease, idiopathic thrombocytopaenic purpura), haematological malignancies (e.g. leukaemia, lymphoma and myeloma), vasculitis, pancreatitis, chemotherapy, endoscopic biopsy or injection [2, 7, 8]. Spontaneous intramural haematoma involves the small bowel in 85% of cases (particularly the jejunum); however, rare cases of isolated oesophageal, gastric, colonic and rectal haematoma have also been described [2]. In contrast, traumatic intramural haematoma usually involves the duodenum due to its relatively fixed retroperitoneal location and close relationship to the lumbar spine [2]. Spontaneous intramural haematomas are generally more extensive, with average length of 23 cm [2].
Clinical presentation of intramural haematoma varies depending on haematoma site and extent and may range from mild non-specific symptoms to severe obstruction and peritonitis [2]. Abdominal pain is the most common presenting symptom and a degree of small bowel obstruction occurs in 85% of cases [2]. The above case was atypical as the patient lacked the classic symptom of abdominal pain. In 40% of cases, rupture of the haematoma results in intraluminal haemorrhage presenting as haematemesis, frank rectal bleeding or malaena [8]. Intramesenteric or retroperitoneal bleeding may also occur, particularly with duodenal involvement [9]. Supratherapeutic INR and leukocytosis are common; however, presence of anaemia is variable, with incidence ranging from 7.6 to 84.6% in case series [3].
Non-contrast abdominal CT is the most valuable imaging modality. Diagnostic features include circumferential bowel wall thickening, intramural hyperdensity, luminal narrowing and intestinal obstruction [2]. Ultrasound is non-specific and may show intra-abdominal free fluid and intestinal wall thickening with an echogenic submucosa [2, 8].
Intramural haematomas are rarely life-threatening and can predominantly be managed non-operatively [3]. As demonstrated above, the mainstay of management is early diagnosis with appropriate resuscitation, reversal of anticoagulation (including anticoagulant cessation, administration of intravenous vitamin K, prothrombinex, fresh frozen plasma or factor concentrates as required) and management of obstructive symptoms [2]. Surgery is advised only for patients with peritonitis at presentation, active haemorrhage, suspected ischaemia, intestinal perforation or deterioration despite medical management [2].
Symptoms typically resolve within 4–6 days of non-operative management [2]. Complete haematoma resorption may take weeks to months; however, it is generally safe to recommence anticoagulant therapy after the acute episode provided it remains within therapeutic limits [2].
Despite its low incidence, intramural haematoma should be considered as a differential diagnosis in anticoagulated patients who present with gastrointestinal symptoms, even in the absence of abdominal pain. This case demonstrates the importance of early diagnosis and the role of non-operative management of an extensive small bowel intramural haematoma.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- anticoagulation
- aortic valve
- anticoagulants, oral
- warfarin
- tachycardia
- abdominal pain
- small bowel obstruction
- intramural hematoma
- differential diagnosis
- international normalized ratio
- intestine, small
- intestines
- signs and symptoms, digestive
- vomiting
- abdominal swelling
- fluid resuscitation
- nasogastric decompression



