-
PDF
- Split View
-
Views
-
Cite
Cite
Qian Wang, Ian Verrall, Rowan Walker, Kevin Tetsworth, Herwig Drobetz, U-type bilateral sacral fracture with spino-pelvic dissociation caused by epileptic seizure, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx043, https://doi.org/10.1093/jscr/rjx043
Close - Share Icon Share
Abstract
Sacral fracture with spino-pelvic dissociation is a rare and unstable injury caused by high-energy trauma, often with serious haemodynamic and neurological implications. Diagnosis is easily delayed or missed as it is often masked by severe associated injuries. Here, we present an unusual case of spino-pelvic dissociation sustained during a seizure episode in a young epileptic patient on long-term anticonvulsant therapy with previous thoracolumbar spinal arthrodesis. This unique case brings to light the need for clinicians to consider sacral fractures in patients presenting with low back pain with no preceding trauma who otherwise may have risk factors for pathological fractures.
INTRODUCTION
Sacral fractures are notoriously underdiagnosed and often undertreated. Despite the potential for neurological compromise, the true incidence of sacral fractures is still unknown [1]. Fractures and dislocations involving the lumbosacral region in healthy adults are usually associated with high-energy trauma [2]. Non-traumatic fractures involving the pelvic region are exceedingly rare, and are often accompanied by additional risk factors such as epilepsy, osteopathy and prior radiation therapy [3].
CASE REPORT
A 37-year-old male presented to a regional emergency department complaining of acute, severe lower back pain following a generalized tonic–clonic seizure lasting 1–2 min. This took place in the passenger seat of a stationary vehicle while he was wearing a seat belt. There was no suggestion of a fall, blunt trauma or any other additional mechanism of injury.
This patient had a background history of a first epileptic fit coinciding with a motor vehicle accident 4 years prior that resulted in T12/L1 burst fracture requiring Harrington rod stabilization from T10 to L3 vertebrae. He had had multiple seizures since then and had been on long-term anti-epileptic therapy, first with carbamazepine then with levetiracetam.
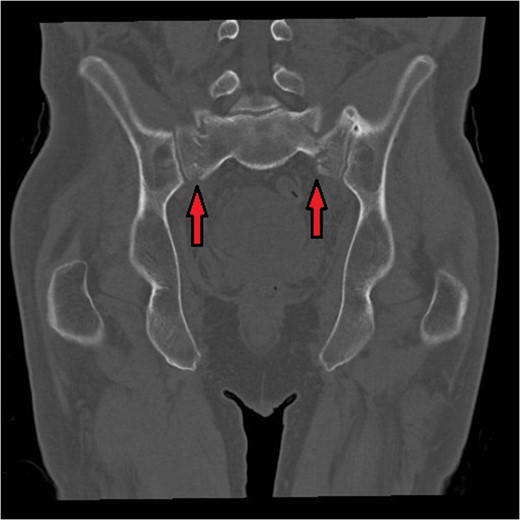
Bilateral sacral fractures (in line with arrows) are clearly visualized on the coronal reformat of CT pelvis.
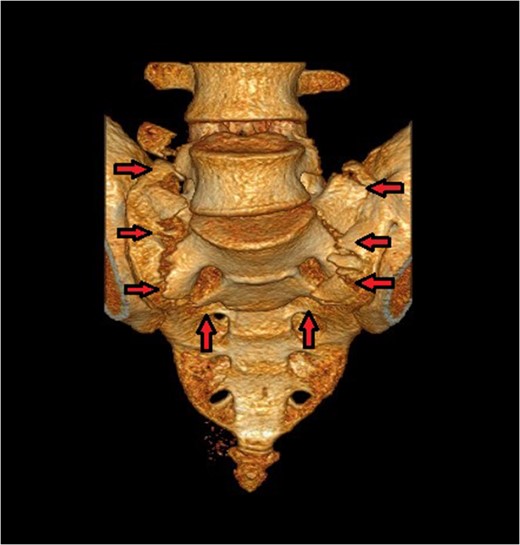
The U-type pattern with spino-pelvic dissociation is better appreciated on the 3D reconstruction of CT pelvis.
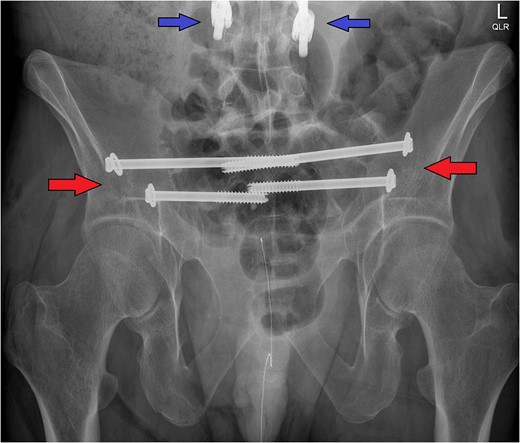
The post-operative X-ray pelvis shows the bilateral ilio-sacral fixation with percutaneous screws (red arrows). Note the inferior portion of the patient's pre-existing thoracolumbar instrumentation (blue arrows) that precluded spino-pelvic fixation as a viable surgical option in this case.
These injuries typically develop a characteristic deformity, with the sacrum and pelvis flexed in relation to the spine [5]. Multiple ilio-sacral screws did not correct the mild deformity already present, but did limit the risk of further progression and allow for early mobilization. Surgery was uneventful, and the patient was immediately much more comfortable. Mobilization was initiated with physiotherapy the following day: partial weight-bearing bilaterally with a frame.
DISCUSSION
Fracture risk is increased in epileptics compared to the general population. While a majority of seizure-related fractures are due to falls and other trauma mechanisms, there is a considerable portion that is non-traumatic in its mechanism and is attributed to the seizure itself [6]. Such fractures have been reported in the spine, the humerus, and, more unusually, in the femur [7]. To the best of our knowledge, this is the first case of a non-traumatic, seizure-induced bilateral sacral fracture with spino-pelvic dissociation. This case, therefore, sheds new light on the amount of force that could potentially be generated during a seizure episode.
There is evidence that anti-epileptic therapy has a dose-dependent effect on increased fracture risk via its effect on vitamin D metabolism and therefore BMD [6]. In the past, anti-epileptic drugs implicated in bone loss included phenytoin, carbamazepine and valproic acid; however, more recent studies that include newer anti-epileptics suggest that levetiracetam may have a greater effect on BMD loss than other agents [8]. There is sparse, underpowered and conflicting evidence on the role of calcium and vitamin D supplementation as a prophylactic measure to reduce fracture risk in patients on long-term anti-epileptic therapy [9]. Further research in this area could better inform clinical decisions regarding pharmacotherapy in epilepsy.
There is growing evidence that sacral insufficiency fractures are a significant potential complication following instrumented spinal fusion [3]. Biomechanical studies have shown spinal fusion to be associated with stress shielding, which can result in localized device-related osteopaenia. The rigid fixation of thoracolumbar instrumentation has also been shown to increase stress during torsion of the spine [10], which may be experienced during epileptic movements. Therefore, sacral fractures must be considered in patients presenting with lower back pain in the context of previous rigid fixation of the thoracolumbar spine. Sacral fractures of this nature may become more common given the increasing prevalence of osteoporosis in an ageing population [3].
In addition to diagnostic challenges, prior instrumented thoracolumbar fusion has potential implications with respect to treatment. If our case had been an isolated fracture, we might have opted for spino-pelvic fixation as the optimal operative management. However, given the biomechanical changes due to the patient's pre-existing thoracolumbar fixation the decision was made to only use ilio-sacral screws. Similar fractures in the past have reportedly been successfully treated with this technique [5].
This case demonstrates that bilateral sacral fracture with spino-pelvic dissociation can occur in the absence of significant trauma, provided there are additional risk factors. Long-term anti-epileptic therapy and associated BMD loss may pose a significant risk for pathological fractures, including those that seem unlikely given the mechanism of injury. Sacral fracture is an increasingly well-documented potential complication in the context of spinal fusion, one that is likely to feature more with the ageing population. Clinicians should, therefore, have a low threshold to further investigate epileptic or post-arthrodesis patients with acute lower back pain whose symptoms are highly suggestive of occult fractures.
CONFLICT OF INTEREST STATEMENT
None declared.



