-
PDF
- Split View
-
Views
-
Cite
Cite
Maria Isaia, Demetris Christou, Panayiotis Kallis, Panayiotis Georgiou, Nikolaos Nikolaou, Panayiotis Hadjicostas, Multiple small intestinal perforations in a patient with Hepatitis B Virus-associated Polyarteritis Nodosa, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx041, https://doi.org/10.1093/jscr/rjx041
Close - Share Icon Share
Abstract
We present the case of a 38-year-old patient with a history of Hepatitis B Virus-associated Polyarteritis Nodosa, who presented with acute abdomen and septic shock. The patient initially had three perforations of the small intestine that were treated with segmental enterectomy and anastomosis at two sites. During his postoperative course he continued to develop new perforations and necrotic lesions along the whole length of the small intestine, that mandated repetitive laparotomies and the technique of the open abdomen was employed. Despite the aggressive surgical treatment and the medical treatment with corticosteroids, cyclophosphamide and plasma exchanges, the patient died 15 days after the first operation due to septic shock and multiple organ failure.
INTRODUCTION
Polyarteritis Nodosa (PAN) is a necrotizing, focal segmental vasculitis that affects medium-sized arteries. Of surgical interest are the gastrointestinal complications that can present as an acute abdomen. These include bowel infarction and perforation, cholecystitis and gallbladder infarction. PAN is associated with Hepatitis B Virus (HBV) in 7% of the cases, and in such cases the incidence of gastrointestinal involvement is higher and the prognosis poorer [1].
CASE REPORT
A 38-year-old male with a medical history of HBV-associated PAN presented with acute abdomen and septic shock. He was diagnosed with PAN 6 months earlier and was under treatment with prednisolone (32 mg daily) and cyclophosphamide (150 mg every other day). The patient was also prescribed the antiviral agent Tenofovir, but stopped taking it 2 months prior to the incident, against medical advice. The patient's medical history also included chronic renal failure and diabetes mellitus Type II. On work up, a standing chest radiograph revealed free sub diaphragmatic air.
During laparotomy, peritonitis was found due to three perforations of the small intestine. Segmental enterectomy with anastomosis was performed at two sites, the first at 10 cm from the ligament of Treitz, and the second at about 1 m from the ileocecal valve.
The patient was then transferred to the Intensive Care Unit on mechanical ventilation and circulatory support, in acute-on-chronic renal failure. On the third postoperative day he was weaned off the ventilator and remained haemodynamically stable. After consultation with the rheumatologist, the patient started treatment with tenofovir orally and IV methylprednisolone 1 gr daily for 3 days.
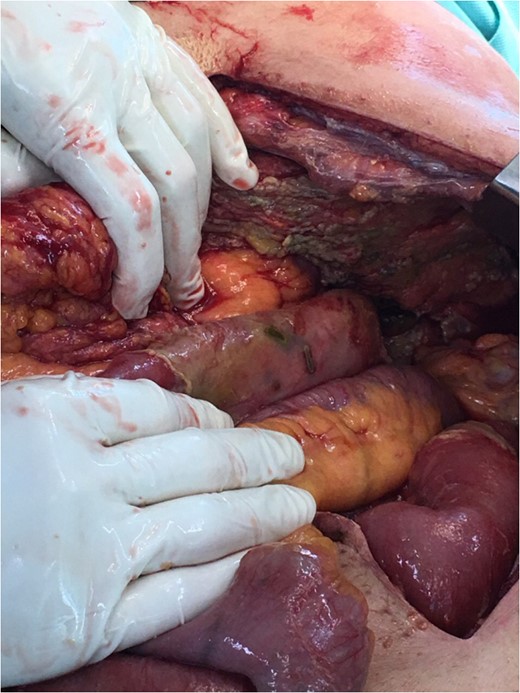
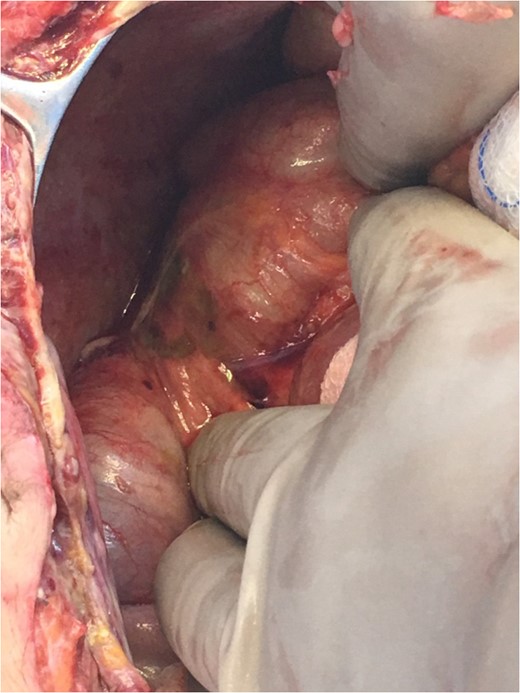
On the seventh postoperative day the patient's abdominal drain catheter presented enteric content, so he underwent a second explorative laparotomy. Two new perforations and multiple areas of patchy necrosis along the whole length of the small intestine were found (Fig. 1). All the lesions were suture repaired after debridement, and the patient was left with an open abdomen using a vacuum device, with a plan for re-laparotomy in 48 h (Fig. 2). After the second operation the patient started plasma exchanges for the treatment of PAN, along with IV cyclophosphamide 500 mg stat and IV methylprednisolone 1 gr daily for 3 days and then IV prednisone 60 mg daily.

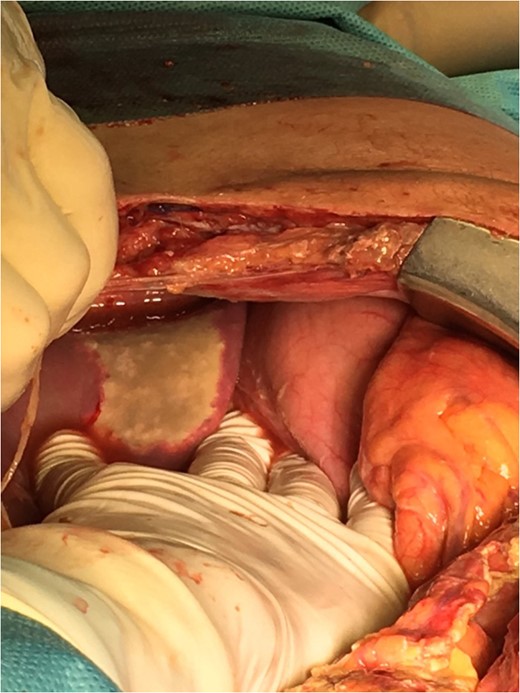
On the third laparotomy, three new necrotic lesions, two on the small intestine and one on the cecum, were found and suture repaired (Fig. 3). A necrotic lesion on the left lobe of the liver was also found (Fig. 4). On the fourth laparotomy, segmental enterectomy with anastomosis and cholecystectomy were performed due to anastomotic leak and a gangrenous gallbladder.
The patient died 15 days after the first operation, despite aggressive treatment, due to septic shock and multiple organ failure.
DISCUSSION
We have presented a case of multiple perforations of the small intestine in a patient with HBV-associated PAN. Our patient was already diagnosed with PAN prior to admission. He reported symptoms that started 1 year earlier and included weight loss, myalgias, fever, skin erythema, deterioration of renal function, new onset of diabetes mellitus Type II and hypertension. The diagnosis of PAN and HBV infection was reached 6 months after the onset of these symptoms. He was under treatment with prednisolone and cyclophosphamide.
According to a protocol for HBV–PAN, the corticosteroids are given for only 2 weeks, as long term use stimulates viral reproduction, whereas rapid discontinuation triggers a rebound of immunologic clearance and favors seroconversion from Hepatitis B e antigen to Anti-HBe antibody. Plasma exchanges are started to remove the immune complexes and an antiviral agent to diminish the viral load [1]. Our patient did not undergo plasma exchanges before presenting with acute abdomen and discontinued taking an antiviral agent against medical advice. Blood tests showed the presence of HBsAg, HBeAg, Anti-HBcAb and the absence of Anti-HBsAb and Anti-HBeAb, which demonstrate HBV infection without seroconversion. A study that compared the evolution of HBV–PAN according to conventional or antiviral treatment showed that when seroconversion was achieved, clinical remission was also obtained and no relapse occurred [2].
Despite medical treatment with corticosteroids, cyclophosphamide and plasma exchanges, our patient's vasculitis remained uncontrolled, as he continued to develop new necrotic lesions and perforations. We tried to control the intestinal complications with repetitive laparotomies. We used the open abdomen technique that was reported to be successful in the management of multiple perforations of the small bowel in another case [3]. Still the patient died 15 days after admission due to septic shock and multiple organ failure, as a result of his uncontrolled vasculitis and immunosuppression.
The prognosis of patients with PAN and severe gastrointestinal involvement is poor. Severe gastrointestinal symptoms, along with renal signs, are the most serious factors of poor prognosis related to PAN [4]. According to another study, peritonitis, bowel perforation, gastrointestinal ischemia or infarctions and intestinal occlusion are associated with higher mortality in patients with necrotizing vasculitides [5]. Gastrointestinal tract involvement is the major cause of death in HBV-associated PAN [2].
The treatment of HBV-associated PAN differs from non-HBV–PAN, because it should also aim to the suppression of HBV replication. This can be achieved with antiviral drugs, combined with plasma exchanges, in order to clear immune complexes which are potentially responsible for the clinical manifestations of the disease [2]. Our patient's PAN was not treated according to this HBV–PAN protocol, and presented with uncontrolled vasculitis that led to multiple perforations of the small intestine.
CONCLUSION
Optimal treatment of HBV-associated PAN as quickly as possible after diagnosis is highly important in order to avoid serious gastrointestinal complications, because once they present the prognosis is very poor, even after aggressive surgical treatment.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- plasma exchange
- polyarteritis nodosa
- acute abdomen
- adrenal corticosteroids
- septic shock
- cyclophosphamide
- glucocorticoids
- hepatitis b
- anastomosis, surgical
- intestine, small
- laparotomy
- necrosis
- surgical procedures, operative
- abdomen
- mineralocorticoids
- viruses
- multiple organ dysfunction syndrome
- small bowel perforation
- medical management



