-
PDF
- Split View
-
Views
-
Cite
Cite
Tatsuya Yamamoto, Yoshiomi Kobayashi, Yoji Ogura, Yohei Takahashi, Yoshio Shinozaki, Jun Ogawa, Delayed leg paraplegia associated with hyperextension injury in patients with diffuse idiopathic skeletal hyperostosis (DISH): case report and review of the literature, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx040, https://doi.org/10.1093/jscr/rjx040
Close - Share Icon Share
Abstract
Diffuse idiopathic skeletal hyperostosis (DISH) is characterized by calcifications and ossification of ligaments and tendon insertions. The patients with DISH are susceptible to spinal column injury with trivial trauma due to immobilization of vertebrae and this easily leads to spinal cord injury. However, only few reports on hyperextension injuries of the thoracolumbar spine with DISH exist. Here we report three cases of those who developed delayed leg paraplegia after hyperextension injuries of the thoracolumbar spine with DISH. All cases complained only lower back pain without neurological deficits and plain radiographs showed no fractures at an initial assessment. The spinal fracture caused by hyperextension injury was diagnosed with computed tomography (CT) and magnetic resonance image (MRI) after delayed leg paraplegia occurred. Many of the fractures caused by hyperextension injuries are not detected only with plain radiographs in patients with DISH. Further investigations using CT and/or MRI should be recommended.
INTRODUCTION
Diffuse idiopathic skeletal hyperostosis (DISH) is non-inflammatory systemic disease which leads to ossification of ligaments and entheses [1]. Especially ossification of longitudinal ligaments causes the ankylosing spine. According to Utsinger, DISH is diagnosed when radiographs present the ossification of at least four contiguous vertebral bodies [2]. Spinal fractures and following spinal cord injuries are easily caused by low-energy trauma in patients with DISH because of immobilized spinal column [3, 4]. The pathogenesis is unknown and the prevalence of spinal DISH varies depending on region and ethnic differences; however, recently an age-related increase in prevalence is undisputed. The type of fracture has a great impact on the prognosis. Several studies suggested that delayed neurological deterioration tends to occur in the fracture caused by hyperextension injury [3]. Here we report three cases of those who developed delayed leg paraplegia after hyperextension injuries of the thoracolumbar spine with DISH.
CASE DESCRIPTION
Case 1
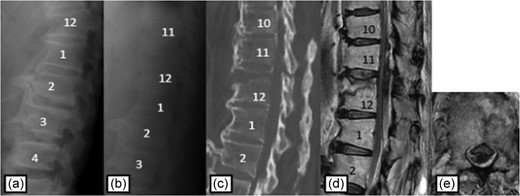
Plain radiographs on initial assessment (a) and on admission (b); Sagittal CT image (c) showing the hyperextension fracture at T12; MRI T2-weighted image (d, e) showing the epidural hematoma compressing the dura matter.
Case 2
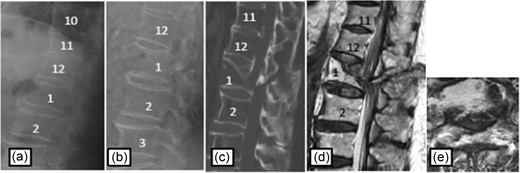
Plain radiographs on initial assessment (a) and on admission (b); Sagittal CT image (c) showing the hyperextension fracture at L1 and dislocation of it; MRI T2-weighted image (d, e) showing the severely compressed spinal cord at L1 level.
| Case . | Mechanism of injury . | Injury level . | Cause of paraplegia . | Duration from injury to paraplegia . | Frankel grade alteration . |
|---|---|---|---|---|---|
| 1 | High energy | T12 | Epidural hematoma | <24 h | C to D |
| 2 | Low energy | L1 | Dislocation | 10 days | B to C |
| 3 | Low energy | L1 | Dislocation | 14 days | A to B |
| Case . | Mechanism of injury . | Injury level . | Cause of paraplegia . | Duration from injury to paraplegia . | Frankel grade alteration . |
|---|---|---|---|---|---|
| 1 | High energy | T12 | Epidural hematoma | <24 h | C to D |
| 2 | Low energy | L1 | Dislocation | 10 days | B to C |
| 3 | Low energy | L1 | Dislocation | 14 days | A to B |
| Case . | Mechanism of injury . | Injury level . | Cause of paraplegia . | Duration from injury to paraplegia . | Frankel grade alteration . |
|---|---|---|---|---|---|
| 1 | High energy | T12 | Epidural hematoma | <24 h | C to D |
| 2 | Low energy | L1 | Dislocation | 10 days | B to C |
| 3 | Low energy | L1 | Dislocation | 14 days | A to B |
| Case . | Mechanism of injury . | Injury level . | Cause of paraplegia . | Duration from injury to paraplegia . | Frankel grade alteration . |
|---|---|---|---|---|---|
| 1 | High energy | T12 | Epidural hematoma | <24 h | C to D |
| 2 | Low energy | L1 | Dislocation | 10 days | B to C |
| 3 | Low energy | L1 | Dislocation | 14 days | A to B |
Case 3
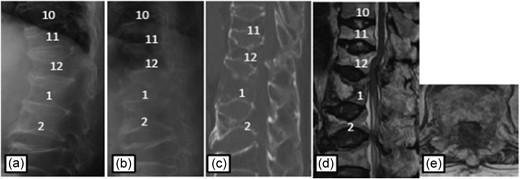
Plain radiographs on initial assessment (a) and on admission (b); Sagittal CT image (c) showing the hyperextension fracture at L1 and dislocation of it; MRI T2-weighted image (d, e) showing the severely compressed spinal cord at T12 level.
DISCUSSION
DISH and ankylosing spondylitis are known as ankylosing spinal disorders, which lead to ankylosis of spinal column. The prevalence of DISH is different between races ranging from 2.9% to 25% [6, 7], and its etiology is unclear. However, several studies showed association with advancing age, obesity and Type 2 diabetes mellitus [3].
DISH patients are susceptible to spinal fracture with trivial trauma due to immobilization of vertebrae. Low-energy trauma caused 32.5–69.1% of fractures [3, 4]. The previous studies reported that most fractures are localized in cervical spine, uncommon at thoracolumbar junction [3, 4, 8]. Hyperextension fracture is the most frequent type of fractures with DISH patients (51.2%) and induces the anterior distraction of vertebral bodies [9]. The fracture spreads transversely resulting in posterior element injuries. Upper and lower fused vertebral bodies make the stress concentration on fracture level, so spinal cord injury due to dislocation of fracture or epidural hematoma is easy to occur after an interval from first injury. Therefore secondary deterioration of neurological status is observed [3, 4, 8]. However, it is difficult to diagnose the hyperextension fracture at the initial assessment only with plain radiograph. Patients with unrecognized fractures commonly complain of only lower back pain until abrupt neurological deterioration occurs. Once after the neurological deficits occur, surgical treatment does not have the great influence to the clinical outcome. Therefore, the definitive treatment should be performed before the second neurological deterioration appears.
The series is summarized in Table 1. We analyzed the mechanism of injury, fracture level, direct cause of leg paraplegia, the duration from onset to paralysis, surgical procedure, and neurological deficits before and after treatment. The mechanism of injury was high-energy trauma in Case 1, and low-energy trauma in Case 2 and Case 3. Fracture level was at thoracolumbar junction in all cases.
The most common cause of spinal cord injury is direct compression by fracture dislocation. Only a few reports mentioned the epidural hematoma causing spinal cord injury [10]. To the best of our knowledge, the timing of second neurological deterioration has not previously been reported. The cause of leg paraplegia was epidural hematoma within 24 h in Case 1, and dislocation of fracture over 1 week in Case 2 and Case 3. The epidural hematoma may be associated with the timing of the spinal cord injury.
A delay in diagnosis often occurs in hyperextension fractures with DISH [3, 4] because it is difficult to diagnose the fractures in plain radiographs due to ankylosing spine. The absence of major trauma may also mislead the diagnosis, this leads to second neurological deterioration.
All cases were treated conservatively at an initial treatment, because the hyperextension injuries in DISH were not recognized only with plain photographs. Further investigation using CT and/or MRI was needed for diagnosis. All patients improved by only one Frankel grade. We can find only a few reports that neurological deficits improved by more than two Frankel grade after surgical treatment [8], again, the definitive treatment should be performed before the second neurological deterioration appears.
CONCLUSION
We here reported three cases of the thoracolumbar hyperextension injuries in patients with DISH, those who developed delayed leg paraplegia. The spinal fracture with DISH is difficult to diagnose only with plain radiograph, therefore screening of spinal column with CT and/or MRI should be recommended even if the fractures are not detected.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- magnetic resonance imaging
- diagnostic radiologic examination
- computed tomography
- diffuse idiopathic skeletal hyperostosis
- fractures
- immobilization
- ligaments
- low back pain
- osteogenesis
- paraplegia
- spinal cord injuries
- tendon
- wounds and injuries
- leg
- spinal fractures
- spine
- hyperextension injuries
- thoracolumbar spine
- vertebrae
- hyperextension
- neurologic deficits
- calcification



