-
PDF
- Split View
-
Views
-
Cite
Cite
Tetsuya Mochizuki, Yuzo Hirata, Shosuke Kitamura, Toshihiro Nishida, Hideto Sakimoto, Laparoscopic operation after pre-operative reduction of an intussusception-induced inflammatory fibroid polyp, Journal of Surgical Case Reports, Volume 2017, Issue 2, February 2017, rjx026, https://doi.org/10.1093/jscr/rjx026
Close - Share Icon Share
Abstract
Intussusception occurs mainly in children but rarely in adults. About 80–90% of adult cases of intussusception are due to benign or malignant neoplasms as a lead point. One of the causes is an inflammatory fibroid polyp (IFP), a rare, benign entity that occurs more frequently in the stomach than the ileum. We describe an uncommon case of a patient who presented with intussusception-induced IFP of the ileum. A 35-year-old woman presented with a 2-day history of abdominal pain. A computed tomography scan demonstrated ileocolic intussusception. During colonoscopy, reduction by pressured air easily released intussusception, and we suspected a submucosal tumour of the ileum. Successful pre-operative colonoscopic reduction was helpful for performing laparoscopic ileocecal resection 2 days later. Results of the histopathological examination confirmed a large IFP. The patient's post-operative course was uneventful. Pre-operative reduction by colonoscopy is effective for the diagnosis and treatment of intussusception-induced IFP.
INTRODUCTION
Intussusception is primarily a childhood disease. Adult intussusception is a rare clinical entity accounting for 5% of all cases of intussusceptions [1]. Intussusception in adults is caused by an identifiable lesion, such as a benign or malignant tumour, as the lead point. Therefore, surgical treatment is often required for intussusception in adults, and it is controversial whether pre-operative and intra-operative reduction of intussusception in adults should be performed [2].
Inflammatory fibroid polyps (IFPs) are rare, benign submucosal tumours of the gastrointestinal tract. IFPs usually arise from the stomach, followed by the small bowel [3, 4]. IFPs are commonly asymptomatic, but they sometimes present with various symptoms, depending on their anatomical location and size. Intussusceptions are one of their clinical conditions associated with IFPs [3, 4].
We describe a patient in whom successful pre-operative colonoscopic reduction for intussusception-induced IFP was very effective in the diagnosis and treatment.
CASE REPORT
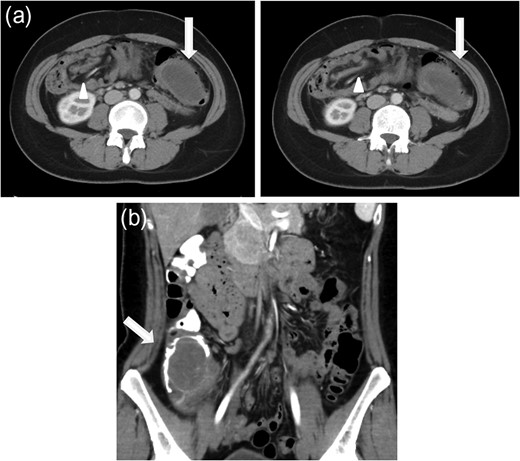
(a) Axial CT scan of the abdomen showing a mass (arrow) filling the transverse colon with accompanying mesenteric fat and vessels (arrowhead) within the lumen. (b) Coronal CT scan after reduction by colonoscopy. A low-density mass (arrow) is pushed back into the caecum.
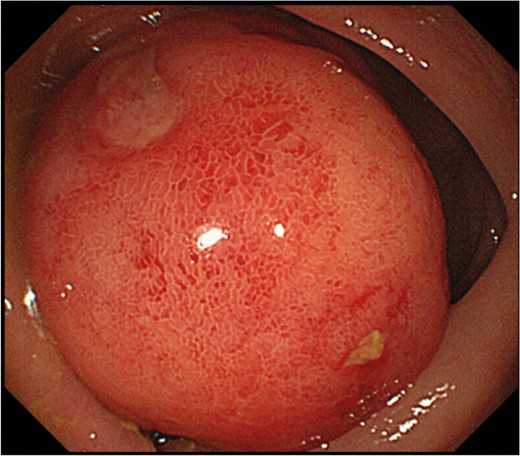
Endoscopic examination showing a pedunculated lesion with the base near the ileocecal valve, occupying most of the transverse colic lumen.
Two days later, a laparoscopic-assisted operation was performed. Her intussusception was almost improved. There was no movable caecum or intestinal oedema; the laparoscopic-assisted operation was performed uneventfully. The ileocecal segment was resected, and functional end-to-end anastomosis was performed.
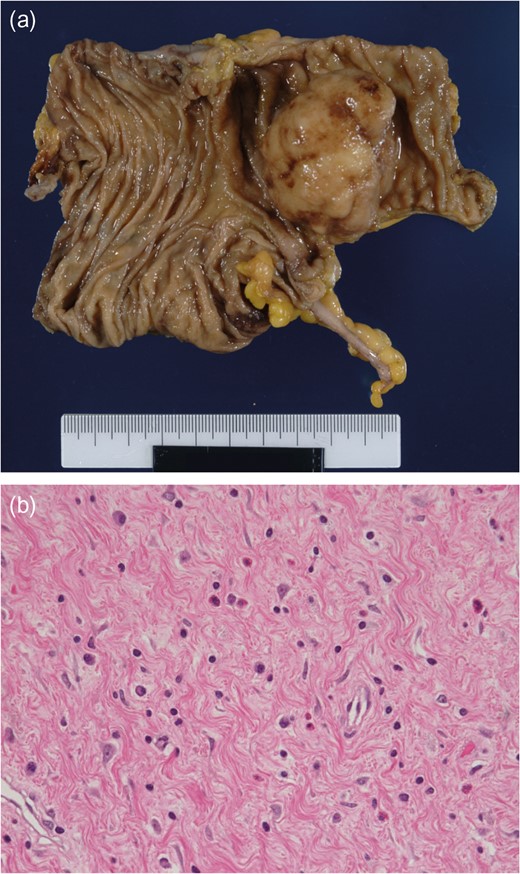
a) The bowel wall is cut away, showing the mass emanating from the ileum. (b) The tumour is composed of bland spindle cells with a fibromyxoid background, containing numerous eosinophils.
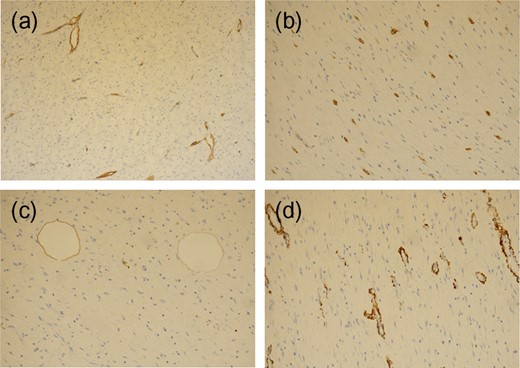
The spindle cells are negatively stained for CD34 (a), C-kit (b), S100 (c) and smooth muscle actin (d).
The patient has had no specific post-operative complications; she was discharged 11 days post-operatively. There was no recurrence at the 8-month follow-up.
DISCUSSION
About 80–90% of adult cases of intussusception are due to benign or malignant neoplasms as a lead point [5]. One of the causes is IFP, a rare, benign submucosal tumour that can occur throughout the gastrointestinal tract [3]. The most common site for IFPs is the gastric mucosa, accounting for ~70% of cases, followed by the small bowel, accounting for 23%, with the ileum predominating [6]. However, the aetiology remains unclear. Some authors have reported that IFPs arise from an allergic reaction against an inflammatory stimulus [3]. Although most patients have a non-specific presentation, those with small intestinal lesions form a symptomatic mass, causing obstruction by intussusception [3]. A definitive diagnosis of IFP is usually based on intra-operative findings [5], and a precise pre-operative diagnosis is very difficult to make.
The treatment of IFPs is resection through an endoscopic or surgical procedure [3]. In the present patient, pre-operative colonoscopy showed that the location of the lesion was the terminal ileum; additionally, an epithelial tumour was ruled out based on endoscopic findings, although no definitive diagnosis could be made with a biopsy. It is important that IFPs, although rare, are considered in the differential diagnosis of adult cases of intussusceptions, especially cases of intussusception-induced submucosal tumour-like lesions.
Pre-operative colonoscopic reduction of intussusception is very effective in its diagnosis and treatment. In children with intussusceptions, the standard therapy is reduction. In adults, however, many studies have pointed out that pre-operative or intra-operative reduction of intussusceptions should not be performed because malignant tumours exist in many cases and there is a possibility of dissemination or haematogenous metastases [3, 5, 7]. Conversely, some authors have emphasized that pre-operative endoscopic reduction may enable physicians to make a qualitative diagnosis and conduct elective surgery after improving intestinal oedema and shortening the length of the intestine to be resected [8]. Furthermore, a better field of view provided by bowel decompression through reduction may facilitate a minimally invasive laparoscopic operation. Intussusceptions are divided into (i) enteroenteric, (ii) ileocecal, (iii) ileocolic and (iv) colocolic types according to where they occur. The enteroenteric type is generally difficult to reduce by performing pre-operative endoscopy because of anatomical reasons, whereas the remaining three types of intussusception are highly likely to be a good indication for pre-operative colonoscopy. Our patient had the ileocolic type. Some authors have reported successful laparoscopic operation in other diseases causing intussusceptions, such as lipoma and hamartoma [9, 10]. In the present patient, we chose to perform pre-operative reduction, because her physical and CT findings indicated no ischaemia or necrosis of the intestines and no peritonitis; the patient underwent a laparoscopic operation without complications.
In the diagnosis and treatment of adult cases of intussusceptions, a laparoscopic procedure after endoscopic reduction could be useful, provided that the patient's condition is tolerable and the surgeon is familiar with performing endoscopic and laparoscopic procedures. However, many published papers have described the reduction of intussusception in a negative manner [3, 5, 7]. When malignancy is strongly considered, a decision to perform reduction needs to be made with caution. More relevant case reports of intussusceptions in adults need to be accumulated in the future.
Pre-operative colonoscopic diagnosis and reduction have advantages, as they help in the decision-making of therapeutic strategies and facilitate the operation, especially the laparoscopic procedure.
INFORMED CONSENT
Informed consent was obtained from the patient included in the study.
CONFLICT OF INTEREST STATEMENT
None declared.



