-
PDF
- Split View
-
Views
-
Cite
Cite
Obteene Azimi-Ghomi, Kamran Khan, Kristian Ulloa, Celiac artery aneurysm diagnosis and repair in the postpartum female, Journal of Surgical Case Reports, Volume 2017, Issue 2, February 2017, rjx010, https://doi.org/10.1093/jscr/rjx010
Close - Share Icon Share
Abstract
A postpartum female presented with aching abdominal pain as well as persistently elevated blood pressure poorly controlled by medication. Computed tomography angiography was performed and identified an aneursym of the celiac artery proximal to its branching points. Due to symptomatic presentation of the patient and plans of future pregnancy, surgical repair of the aneursym was planned and performed 2 months following initial diagnosis. Celiac artery aneurysms are rare types of visceral artery aneursyms (VAAs) and comprise ~4% of all VAAs.
INTRODUCTION
Visceral artery aneurysms (VAAs) are an uncommon finding usually diagnosed in pregnant and postpartum females. Due to their tendency to be asymptomatic as well as their potential to rupture and lead to significant mortality in this patient group, once diagnosed, they are typically promptly repaired surgically or endovascularly. Celiac artery involvement is a rare presentation of VAA and a challenge to repair due to its location and associated branching arteries.
CASE REPORT
A 34-year-old Liberian woman G2P2002 presented to us from the Obstetrics Department 9 days postpartum complaining of nausea, vomiting and epigastric discomfort. Her pregnancy was complicated by oligohydramnios and severe pre-eclampsia with reported systolic BP in the 200s. The patient was treated with magnesium sulfate, labetalol, hydralazine, nifedipine and underwent a Caesarian section delivery at 41.2 weeks. Prenatal care was split between the USA and Liberia. The patient denied any previous complications with the first pregnancy, which was delivered at term vaginally. Physical examination of the patient demonstrated uterine fundus at the level of the umbilicus but was otherwise benign.
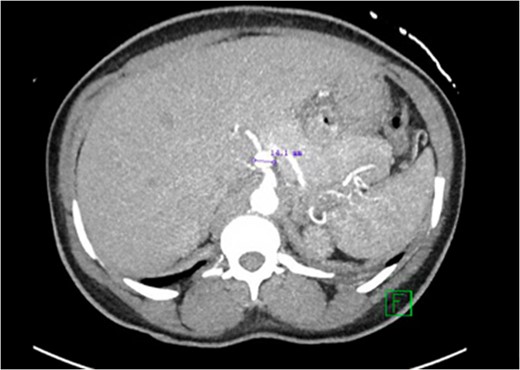
CT abdomen with contrast demonstrating the location and size of the aneurysm.
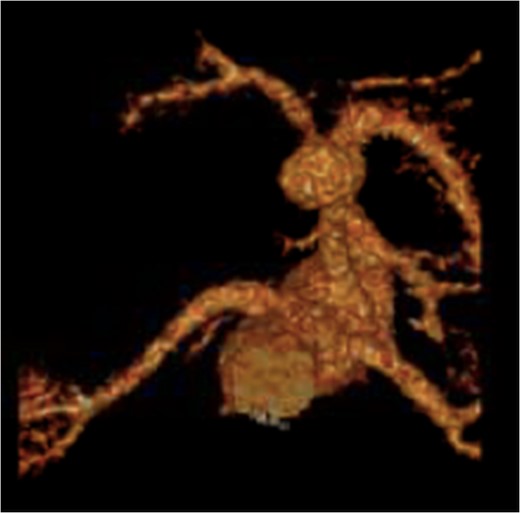
Recreated 3D imaging of the aneurysm arising from the ventral aspect of the distal celiac artery.
The patient was educated on her elevated risk of aneurysm rupture due to her childbearing age, and also advised on the high risk of rupture should she become pregnant again. The decision was made to follow-up with the patient in outpatient vascular surgery clinic for ongoing aneurysm surveillance and planning for surgical repair.
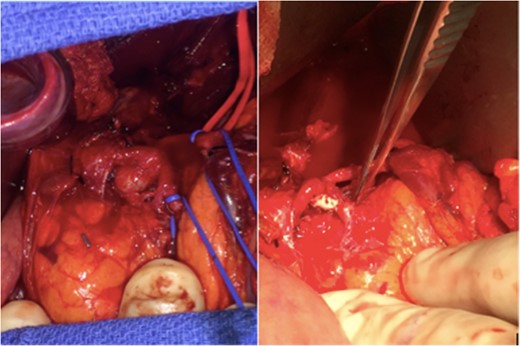
Intra-operative image demonstrating the anerusym in situ before repair (left) and the vascular patch repair following aneurysm removal (right). The pancreas is located inferior to the celiac artery in this image.
The patient's postoperative course was uncomplicated and lasted a total of 3 days. Patient's bowel functioning returned within 24 h of the operation and she was able tolerate PO intake on postoperative day #2. No further complications were reported by the patient and she is to follow-up in clinic at 3 months postoperative.
DISCUSSION
VAAs are an uncommon phenomenon that is usually asymptomatic and go undiagnosed in the majority of affected patients. They are commonly discovered incidentally on CT abdomen or CT angiography. They are however of great concern due to their potential for possible rupture resulting in life-threatening hemorrhage. Approximately 22% of diagnosed VAAs undergo rupture, with an associated mortality rate of 8.5% [1].
VAAs most commonly involve the splenic artery (60%) and hepatic artery (20%). Less commonly involved visceral arteries are the superior mesentery artery (5.5%), celiac artery (4%), gastric and gastro-epiploic arteries (4%), jejunal/ileal/colic arteries (3%), pancreatico-duodenal and pancreatic arteries (2%), gastroduodenal artery (1.5%) and inferior mesenteric artery (<1%) [1]. Celiac artery aneurysms are commonly seen in the setting of atherosclerosis and medial degeneration [2].
The underlying pathophysiology in the development of VAAs is unclear but has been associated with atherosclerosis, cystic medial degeneration, trauma, infection/inflammation and conditions of increased blood flow through the visceral vasculature (e.g. pregnancy, portal hypertension, liver transplant patients). Pregnancy is associated with 20–50% of all VAA ruptures [3, 4].
VAAs are usually asymptomatic; if symptomatic, clinical symptoms and signs vary depending on the location of the aneurysm, and are often nonspecific and include malaise, vague abdominal pain, nausea and/or vomiting. Due to the rarity of VAA, they are typically not suspected initially as the cause of the patient's symptoms and diagnosis can therefore be delayed. A ruptured VAA can present with abdominal pain due to an expanding hematoma, or signs of free intra-abdominal bleeding (e.g. tense abdomen, hemodynamic instability). Physical examination is often of little help in the diagnosis of VAA and laboratory studies may be normal or nonspecific. Ultrasonography and cross-sectional abdominal vascular imaging (CT angiography or magnetic resonance imaging) usually provide accurate diagnosis of VAA.
Treatment of VAA depends on: symptomatology, size, rate of expansion, pregnancy or childbearing status, and future orthotopic liver transplantation. Currently accepted recommendations for repair of VAA include [5, 6]:
- Symptomatic aneurysm
- 2 cm in diameter
- Rate of expansion >0.5 cm/year
- Asymptomatic VAA in pregnant women or any women of childbearing age
- Asymptomatic VAA in patient undergoing orthotopic liver transplantation
Celiac artery aneurysms can often be repaired by open surgical repair via a transabdominal approach [7]. Artery ligation may be performed if the patient does not have concomitant liver pathology due to elevated risk of hepatic ischemia from this procedure [7]. Endovascular management may be appropriate in high-risk patients.
Complications of VAA repair include: coil migration resulting in fatal GI hemorrhage, ischemic gastritis, gastric or duodenal ulcers, gangrenous cholecystitis, liver abscess and exacerbation of cirrhosis [8].
CONFLICT OF INTEREST STATEMENT
None declared.



