-
PDF
- Split View
-
Views
-
Cite
Cite
Elio Treppiedi, Giuseppe Zimmitti, Alberto Manzoni, Valentina Sega, Francesca Guerini, Stefano Mutti, Mariano Lombardi, Tamu Bonaventure, Edoardo Rosso, Extra peritoneal giant pelvic hibernoma: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx250, https://doi.org/10.1093/jscr/rjx250
Close - Share Icon Share
Abstract
Abdominal hibernoma is a rare slow-growing tumor originating from brown adipose tissue. Due to its rarity, only a few case reports have been published so far. Pelvic localization is anedoctal and preoperative differential diagnosis with other malignancies may be challenging. We present the case of a woman who, due to a lower abdominal pain, underwent an abdominal ultrasonography with diagnosis of a 15 cm hyperechogenous pelvic mass. A subsequent MRI showed a 16 × 5.8 × 7.8 cm3 lesion anterior to the left iliacus muscle, with an intra- and extrapelvic component longitudinally extending from the left anterior superior iliac spine until the lesser trochanter. Surgical resection was performed and final histopathology was consistent with hibernoma. This report emphasizes the necessity to include hibernoma among differential diagnosis when a retroperitoneal abdominal mass is diagnosed and the difficulty to perform preoperatively this diagnosis due to the extreme rarity of these neoplasms.
INTRODUCTION
Hibernoma is a rare benign tumor firstly described by Merckel in 1906, but named by Gery in 1914 [1]. It originates from brown fat, has been reported only in a few articles and morphologically mimics the brown fat of hibernating animals [2].
When facing hibernoma, it is of utmost importance to adequately differentiate it from soft-tissue originating malignant tumors, as liposarcoma where an aggressive treatment is justified; in this context, CT scan and MRI may help in differential diagnosis.
CASE REPORT
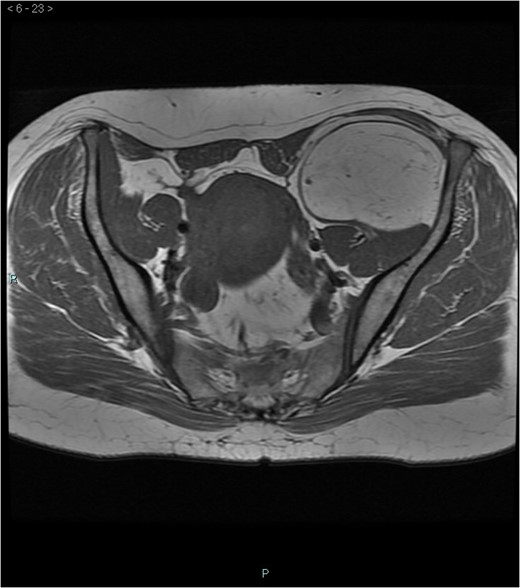
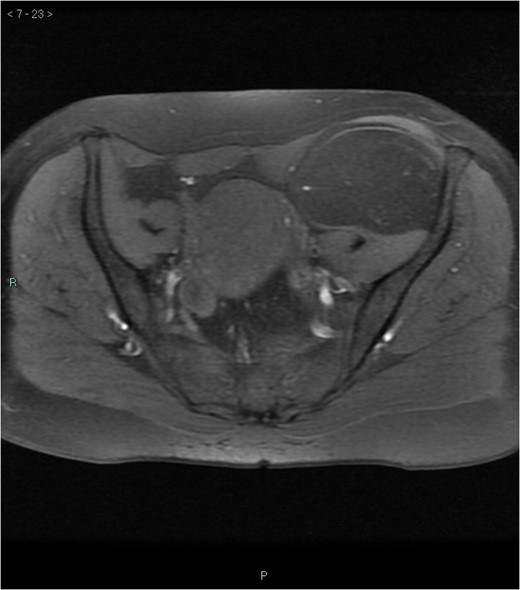
A 58-year-old woman was evaluated for lower abdominal pain, without additional symptoms. An abdominal ultrasonography revealed the presence of a 15 cm homogenous mass, located in the left pelvic cavity. Subsequent MRI showed a capsulated mass, isointense with the adipose tissue, longitudinally extending from the left inguinal area to the left leg root and located on the medial aspect of the left iliac bone. MRI also revealed within the mass some fibrotic branches containing small blood vessels. No evidence of extracapsular invasion of the surrounding structures was evident (Figs 1–6).




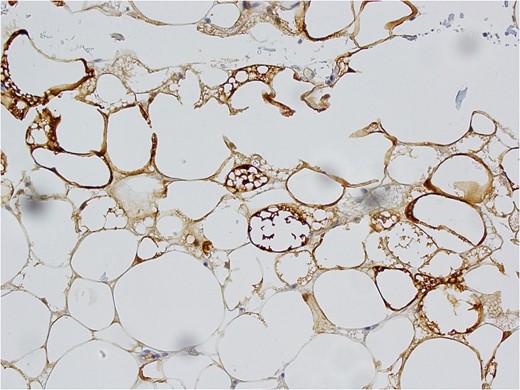
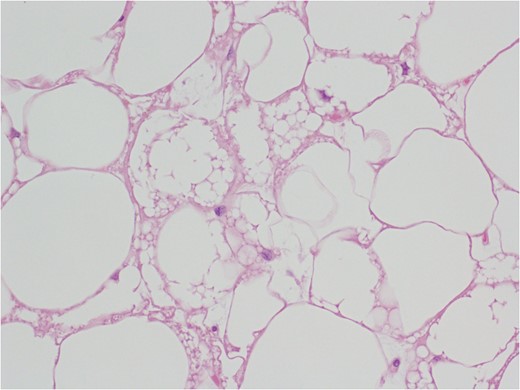
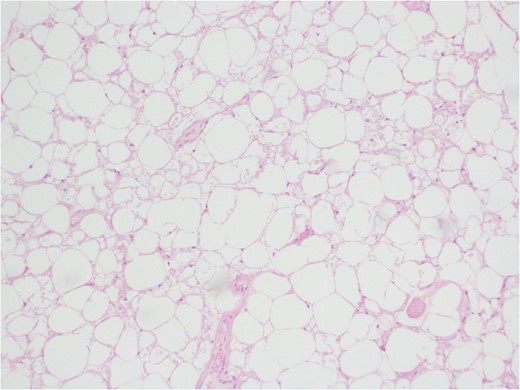
After multidisciplinary team discussion, surgical resection of the mass was planned: through a Pfannestiel incision a retroperitoneal dissection was performed, until exposition of the overmentioned mass, which was completely enucleated. During the operation, the absence of tumor infiltration of the surrounding structures was confirmed. No intraoperative histopathologic examination was carried out and the lesion was sent for definitive pathological examination. Macroscopically, the tumor presented as a well circumscribed encapsulated soft mass without infiltrative growth and/or satellite nodules. Tumor size was 15 × 7.5 × 6.5 cm3 and the weight was 309 g. External surface was smooth and the section had a lobulated aspect with a yellow-brown color. The histopathology examination revealed an adipocyte proliferation with moderate volume variation. Two populations of adipocytes were identified: one cluster with small, bland nuclei and the other with round to oval nuclei, with vacuolated eosinophil cytoplasm. In addition, rare multinucleated giant cells were observed. No cellular atypia was present. Immunohistochemistry was positive for S-100 and negative for MDM-2 (murine double-minute type 2) (Figs 7–9). Postoperative course was uneventful and the patient was discharged after 2 days.
DISCUSSION
Hibernoma is a benign and slowly growing soft-tissue tumor containing brown fat. It develops in the context of the anatomical space where brown adipose tissue is present. Adipose tissue was first described in 1670 by Welch in hibernating animals and it is believed to represent a kind of fetal fat whose function is to promote nonshivering thermogenesis, gradually replaced by white adipose tissue with human development [3].
Diagnosis is incidental in the majority of cases and occurs during radiologic investigations performed for other conditions but rarely may be due to symptoms linked to the mass effect.
According to the largest available series of hibernoma published so far [2], the most common anatomic locations include the thigh or the upper thorax, while the pelvic location is quite rare. Hibernoma are usually diagnosed in the third or fourth decades of life while it is rare in old or in pediatric patients with a slight female predominance described. Different histological variants have been described, the most frequent being those containing eosinophilic cells, pale cells and mixed cell types, similar to our case [2]. Genetically, unlike others benign lesions originating from fat tissue, hibernoma cells present several cytogenetic rearrangements, typically translocations and cromosome breaks, supposed to be involved in the pathogenesis of this tumor [4].
Preoperative differential diagnosis is mainly based on radiologic imaging and is very difficult, because no pathognomonic signs exists for diagnosis of hibernoma; usually CT-scan shows an homogenous lesion, whose density is between subcutaneous fat and skeletal muscle; MRI shows slightly lower signal intensity on T1 weighted spin-echo (T1WSE), marked enhancement and partial fat suppression on short Tau inversion recovery (STIR) and fat-saturated sequences [5].
Usually, metabolic evaluation with FDG PET shows an intense FDG uptake miming a neoplastic lesion like liposarcoma or metastases [6–8]. The histological reason of this false positive effect could be related to an increased numbers of mitochondria, causing an high rate of glucose metabolism.
Finally our report shows an atypical localization of a rare benign tumor. Its rarity and the uncertainty of the preoperative diagnosis confirm that hibernoma represents a clinical challenge for surgeons, pathologists and radiologist. Complete excision of the tumor still represents the treatment of choice.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- magnetic resonance imaging
- abdominal mass
- cancer
- brown fat
- differential diagnosis
- preoperative care
- retroperitoneal space
- abdomen
- diagnosis
- neoplasms
- pelvis
- peritoneum
- pelvic mass
- hibernoma
- iliacus muscle
- abdominal ultrasonography
- abdominal pain, lower
- excision
- lesser trochanter of femur
- Anterior superior iliac spine
- histopathology tests



