-
PDF
- Split View
-
Views
-
Cite
Cite
Mark Magdy, Hyerim Suh, Vytauras Kuzinkovas, Novel technique using a bioabsorbable prosthesis with fibrin glue fixation to prevent a Petersen’s space hernia, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx246, https://doi.org/10.1093/jscr/rjx246
Close - Share Icon Share
Abstract
Introduction: Laparoscopic Roux-en-Y gastric bypass is a bariatric operation that is effective for long-term weight loss. Although rare, one serious complication is an internal hernia through Petersen’s space, which may result in bowel strangulation. Although the incidence of internal hernia can be reduced through closing the Petersen’s defect, it does not eliminate the risk. This case describes a novel and reliable method to close Petersen’s defect. We report the case of a 30-year-old female who underwent a laparoscopic Roux-en-Y gastric bypass for the management of morbid obesity. Following her Roux-en-Y reconstruction, a prosthetic bioabsorbable mesh was placed in Petersen’s space and reinforced with fibrin glue to prevent internal herniation through Petersen’s defect. The use of a bioabsorbable mesh in Petersen’s space is a novel and easy technique that could be used to reduce the incidence of an internal hernia through Petersen’s defect.
INTRODUCTION
Laparascopic Roux-en-Y gastric bypass (RYGB) is favoured over the open approach as it is safer and more effective, with a mortality rate of 0.5% and morbidity around 7–14%[1]. One advantage is that patients develop fewer post-operative adhesions. However, the main cause of late post-RYGB complications is the development of internal hernias such as a Petersen’s hernia [2]. This has been attributed to the lack of post-operative adhesions after a laparoscopic operation and potentially increased mobility of the small bowel [2, 3]. The overall incidence of internal hernias ranges from 1 to 4%, with the majority occurring at the Petersen’s defect and enteroenterostomy site [3–6]. The incidence is lower in open gastric bypasses, however, open surgeries carry the risk of small bowel obstruction secondary to adhesions [7].
Petersen’s hernia is a type of internal hernia that occurs most frequently after a laparoscopic RYGB. During the procedure, a space between the alimentary loop of the small bowel and the transverse mesocolon is created and is called the Petersen’s defect. Subsequently a part of the small bowel can herniate through this orifice. As this operation is becoming more common, the incidence of internal herniation has been increasing [2]. Although it is a relatively rare complication, it can be potentially life threatening due to the risk of bowel strangulation and gangrene [8]. Diagnosis is difficult as patients can present months or years after the procedure with non-specific symptoms, clinical findings and imaging [9]. Closing the defect with sutures can prevent this complication, but that approach in an obese patient can be technically challenging and has suboptimal results. Through this case report we present a novel technique utilizing a prosthetic bioabsorbable mesh to close Petersen’s defect.
CASE REPORT
We present a case of a 30-year-old female with a body mass index (BMI) of 37.2 kg/m2 who was admitted to St. George hospital for a laparoscopic RYGB for the management of morbid obesity. The patient previously underwent laparoscopy for endometriosis with a background of non-insulin dependent diabetes, depression and hypertension.
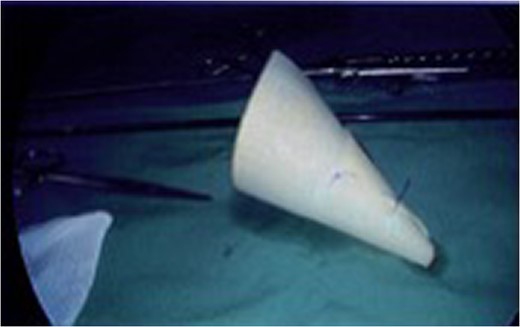
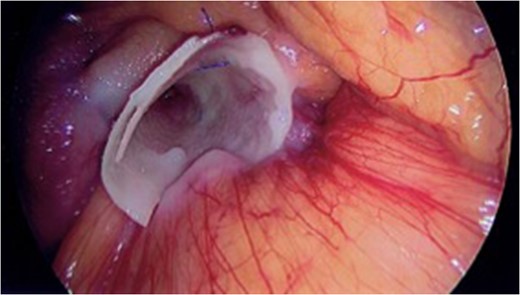
A standard Laparoscopic Roux-en-Y bypass was performed, where the gastric pouch was created with an endoscopic stapler. Following this, the jejunum was transected and an antecolic single layer handsewn gastroenterostomy was performed. A single layer handsewn enteroentrostomy was then performed. Petersen’s space was then inspected as per Fig. 1. Following this procedure, a 1 mm Gore BioA Tissue Reinforcement (HH0710) was rolled into a funnel then sutured in position with a 3-0 prolene suture as seen in Fig. 2.

Photograph of Peterson’s defect laparoscopically following Roux-En-Y gastric bypass.
The shaped prosthetic mesh was secured over Petersen’s defect with fibrin glue (Tisseel) (Fig. 3). The Petersen’s defect was identified as the space between the jejunum (Roux limb) and the transverse colon. The reinforcement of the defect was substantial and the average time taken to place the mesh was 5.0 min. The patient made an uneventful post-operative recovery.
DISCUSSION
Laparascopic RYGB has been favoured over the open surgery as it is safer and more effective with a lower mortality rate of 0.5% [1]. One of the advantages is that patients present with fewer post-operative adhesions. However, the main cause of late post-operative complications is the development of internal hernias such as a Petersen’s hernia in patients treated with this technique [2]. The overall incidence of internal hernias ranges from 1 to 4%, with the majority occurring at the Petersen defect and enteroenterostomy site [3–6].
In normal anatomy the transverse colon and its mesentery functions as a division between the stomach and the small intestine. However, by creating a gastro-jejunal anastomosis, this natural partition is disrupted, creating the potential for an internal herniation such a Petersen’s hernia [5]. The boundaries of a Petersen’s hernia are the transverse mesocolon, the Roux limb and the retroperitoneum. Essentially the small bowel herniates into the space between the cut Roux limb mesentery and the transverse mesocolon. This can result in serious complications such as bowel necrosis secondary to strangulation as well as superior mesenteric vein obstruction with twisting of the intestines [4, 5, 7].
Evidence for the risk factors for a Petersen’s hernia are conflicting. Some report that the antecolic placement of the Roux limb has a higher incidence than retrocolic but the converse has also been observed [4]. Furthermore, the weight loss and associated decrease in abdominal fat can also increase the size of the mesenteric defect, increasing the risk for herniation [5].
Diagnosis of internal hernia into the Petersen defect is challenging as patients can present with normal laboratory values, non-specific physical examination findings and non-diagnostic imaging results [8, 9]. The most common presentation are signs of small bowel obstruction that include intermittent abdominal pain (from recurrent herniation), nausea and vomiting [4]. Furthermore, sometimes the herniation can self-resolve, which also delays the diagnosis [2].
Therefore, the clinician must have a high index of suspicion for patients presenting with abdominal pain after a gastro-jejunal anastomosis. An abdominal CT is the most accurate imaging technique, where it may reveal abdominal distension, herniation and rotation of mesenteric arteries and veins [10]. However, positive CT findings are only present in 74% of patients with internal herniation through Petersen’s defect [1], thus the diagnosis can only be confirmed by an exploratory laparoscopy [2, 4].
Treatment of an internal hernia through the Petersen defect is by reducing the hernia and closing the mesenteric defects with sutures [5]. In cases with severe bowel strangulation; gastric, small bowel and colonic resection may be necessary [9]. However, there is a lack of data regarding the prevention of a hernia in Petersen’s space, and according to literature, this is the first report on the use of an absorbable mesh to prevent this feared complication.
CONFLICT OF INTEREST STATEMENT
There are no conflicts of interest to declare.
ETHICAL APPROVAL
Written informed consent was obtained from the patient in regards to the publication of this case report and associated images.



