-
PDF
- Split View
-
Views
-
Cite
Cite
Nolan R Bruce, Jacob T Carlson, Kayla J Barnard, Ronda Henry-Tillman, Phyllodes tumor masquerading as a fungating breast mass, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx220, https://doi.org/10.1093/jscr/rjx220
Close - Share Icon Share
Abstract
Phyllodes tumor of the breast is an uncommonly encountered disease. The tumor presenting as fungating breast mass or ‘ruptured’ breast is an even more rare presentation of an unusual disease. This report documents the case of a 60-year-old female with delayed presentation of a large exophytic mass of the left breast. Biopsy of this lesion was non-diagnostic, so excision via left total mastectomy was performed. The final pathology was consistent with malignant phyllodes tumor. This report highlights the features of a rare breast cancer, the challenges in obtaining a definitive diagnosis, and the treatment of this disease, in an effort to provide clinicians with an example of the management of such a peculiar entity.
INTRODUCTION
Phyllodes tumors are rare fibroepithelial tumors that comprise <0.5% of breast malignancies [1], uncommonly encountered even by those who specialize in the treatment of breast cancer. Only 500 cases of phyllodes tumor are diagnosed annually in the USA [2]. These tumors are classified as benign, borderline or malignant based on histologic features, which include stromal cellularity and atypia, mitotic index, infiltrative margins and stromal overgrowth. Of these features, stromal overgrowth is considered the most predictive of the malignant potential [2]. Phyllodes tumors are considered malignant if they demonstrate: a high mitotic index with sarcomatous stromal atypia, or stromal overgrowth with either a high mitotic index or sarcomatous stromal atypia.
The diagnosis of phyllodes tumor can be difficult to determine pre-operatively, which underscores the importance of excising any lesion that remains suspicious in an astute clinician’s judgment. These tumors can be identified either as a palpable mass or an abnormality on radiographic imaging. Unfortunately, the hallmark radiographic findings of a phyllodes tumor are similar to those of benign entities, such as the smooth, well-circumscribed appearance of a fibroadenoma. Large size (>3 cm) or rapid growth of any ‘fibroadenoma’ on imaging should immediately raise suspicion for a phyllodes tumor. Core needle biopsies or fine needle aspirates (FNA) are often misleading [3] and may not definitively diagnose a phyllodes tumor. Identifying specific cytologic features (fibromyxoid stromal fragments with spindle nuclei, fibroblastic pavements and spindle cells of fibroblastic nature) on FNA can increase the diagnostic yield. The diagnosis largely relies on clinical suspicion and is often not determined until the pathology of the surgically excised lesion is reviewed.
The standard of care for treatment of phyllodes tumor entails complete surgical excision. There is no difference in recurrence rate between appropriate wide local excision or mastectomy, though surgical margins of <1 cm have been associated with higher rates of local recurrence and worse outcomes [4]. Phyllodes tumors most commonly metastasize via hematogenous spread; thus, there is no role for axillary lymph node dissection for staging of these tumors. Utilization of adjuvant radiation in treatment of phyllodes tumors is currently evolving. Local recurrent rates have been shown to decrease with the administration of adjuvant radiation therapy for borderline or malignant tumors following wide local excision [5]. Metastatic disease should be resected when feasible. Presently there is no consensus data that supports the use of systemic chemotherapy for metastatic phyllodes tumors. Current chemotherapy guidelines for this malignancy have been extrapolated from guidelines for treatment of soft tissue sarcomas.
CASE REPORT
A 60-year-old female presented to the emergency room with ‘rupture’ of the left breast. She had felt a mass in her left breast with tenting of the overlying skin ~1 year prior to presentation but never sought treatment due to lack of insurance. The mass continued to increase in size over the ensuing year. She elected to seek evaluation when the mass eroded through the overlying skin and began to bleed.
Physical exam revealed a large fungating mass extruding from the left breast at the 3 o'clock position with overlying ulceration and cellulitic changes to the surrounding skin (Fig. 1). CT scan of the chest demonstrated a 9.2 × 8.6 cm heterogeneous mass in the left breast with reactive lymphadenopathy up to 3.1 cm in the ipsilateral axilla (Fig. 2). There were no suspicious findings in the right breast on CT and mammographic imaging (Fig. 3). MRI of the brain demonstrated no evidence of metastatic disease. Core needle biopsy (CNB) of the mass demonstrated focal granulomatous reaction with foreign body giant cells. CNB of the enlarged axillary node was benign.

A large fungating mass was found to have ‘ruptured’ through the lateral left breast.
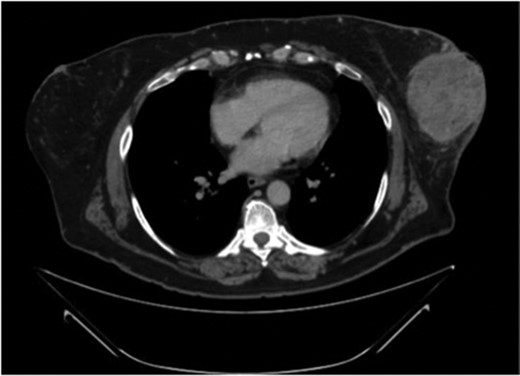
CT scan of the chest demonstrates a 9.2 × 8.6 cm mass within the left breast causing ulceration of the overlying skin.
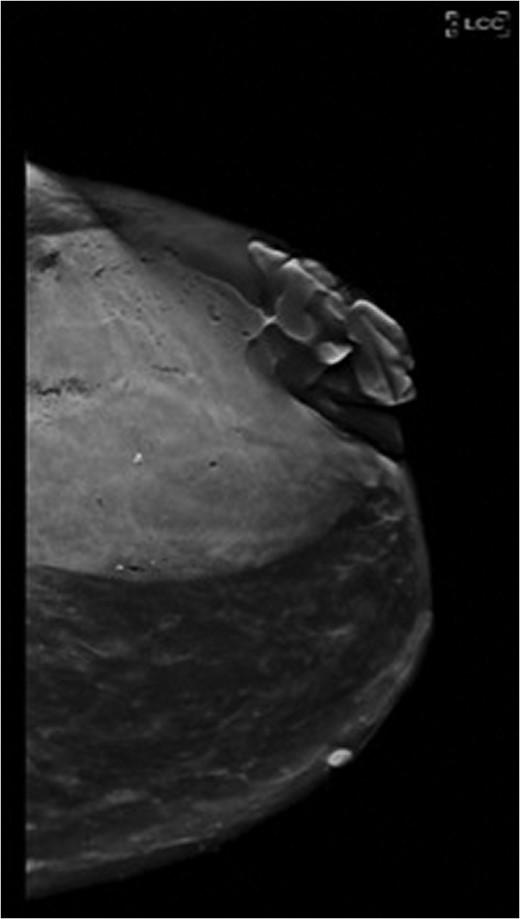
Craniocaudal view of the left breast on mammography demonstrates the extent of the fungating mass.
Due to the size of the mass and strong concern for malignancy, the patient elected to proceed with left simple mastectomy (Fig. 4). Intra-operative analysis of an incisional biopsy of the mass remained inconclusive. Final pathologic analysis of the mastectomy specimen determined the lesion to be a phyllodes tumor with significant stromal overgrowth, measuring up to 9.5 cm. The mass was completely excised with margins >2 cm on each surface. Due to the significant stromal overgrowth and cellular morphology on histology, this was classified as a malignant phyllodes tumor. The patient’s post-operative course was uncomplicated, and she was discharged on post-operative day 1. The patient had no evidence of disease on follow-up. Adjuvant radiation treatment was recommended, but the patient deferred this option.

The left breast mass was excised with >2 cm margins in the left breast mastectomy specimen.
DISCUSSION
This case report documents the unique presentation of a rare breast tumor. Phyllodes tumors can distort the architecture of the breast causing pressure necrosis of the overlying skin, resulting in ‘rupture’ of the breast. Fungating breast masses are more commonly due to invasive ductal carcinoma (IDC) that has invaded the epithelium. The classic presentation of IDC is a mass that is contiguous with the infiltrated skin and everted edges. Phyllodes tumors, on the other hand, is associated with an exophytic mass that pushes the skin borders outward and causes skin loss due to pressure necrosis, creating a skin shelf surrounding the extruding tumor. As seen in this case presentation, phyllodes tumors can be difficult to diagnose on needle biopsy, which highlights the need for excision of any suspicious or rapidly enlarging masses. Local recurrence rates are generally low following surgical resection with margins >1 cm (4.3% for benign tumors and 12.8% for borderline and malignant tumors) [6]. Overall, 5-year survival for patients with a phyllodes tumor is generally favorable following surgical resection: 96% for patients with benign tumors, 74% for patients with borderline tumors and 66% for patients with malignant tumors [6]. Of the pathologic features associated with malignancy, stromal overgrowth most closely correlates with mortality [4]. This article describes the unique presentation of a phyllodes tumor and emphasizes the obstacles and decisions posed to the clinician in the management of such an uncommon breast mass.
ACKNOWLEDGMENTS
The authors would like to acknowledge the University of Arkansas Departments of General Surgery and Breast Oncology for their support and assistance in the writing of this case report.
CONFLICT OF INTEREST STATEMENT
None declared.



