-
PDF
- Split View
-
Views
-
Cite
Cite
Masahiro Shiihara, Wataru Izumo, Ryota Higuchi, Takehisa Yazawa, Shuichiro Uemura, Toru Furukawa, Masakazu Yamamoto, A case of long-survival insulinoma with multiple neuroendocline tumour type 1 controlled by multimodal therapy, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx244, https://doi.org/10.1093/jscr/rjx244
Close - Share Icon Share
Abstract
Insulinomas with multiple neuroendocrine tumour type 1 (MEN1) sometimes have metachronous or recurrent tumours. However, the treatment for these tumours is controversial, and published reports regarding multimodal therapy for insulinomas are limited. We report a 73-year-old woman with recurrent insulinoma with MEN1 successfully controlled by multimodal therapy. She had several complications, and poor performance status. Her hypoglycaemia did not improve after 6-month octreotide LAR; as such, she underwent enucleation of the pancreatic tumour. Within 7 years after the first operation, she underwent four succeeding surgeries for recurrent tumours. Her medications during follow-up were octreotide-LAR and Everolimus. Insulinoma can be managed through various treatment options. Medical treatment includes octreotide-LAR and Everolimus, while surgical approach includes enucleation and pancreaticoduodenectomy. Some tumours, particularly those that are MEN1, can recur repeatedly. Thus, several treatments are needed to control them. We highlight the importance of multimodal therapy, including repeated surgery, for the control of the disease.
INTRODUCTION
Insulinoma is commonly a benign tumour but can sometimes have malignant factors. In particular, patients with multiple neuroendocrine tumour type 1 (MEN1) sometimes have metachronous tumours or recurrent insulinomas. Thus, patients with insulinoma require multimodal therapy, including repeated surgery, to achieve long-term survival. However, reports regarding multimodal therapy for insulinoma are limited.
CASE REPORT
A 73-year-old woman who had Whipple’s triad for a year presented to our hospital and sought consultation.
She had multiple complications, including chronic renal failure, atrial flutter, primary hyperparathyroidism, hypertension and Cushing syndrome, and underwent hemi-thyroidectomy at 59 years of age for hyperparathyroidism. Her family history was not remarkable.
Physical examination revealed central obesity and moon face with normal vital signs. Her body mass index was 24.6 kg/m2, and alopecia and pitting oedema of the legs were detected.
The fasting serum glucose level measured 31 mg/dl, while insulin level was elevated to 33.5 μU/ml. The serum insulin level remained high after glucose loading. However, her serum ACTH level was within normal limits at 12.2 pg/ml, and her dexamethasone suppression test was negative. The serum intact-PTH level was elevated to 596 pg/ml, but the calcium level was within normal limits at 9.5 mg/dl. The free-T3 and free-T4 levels were slightly elevated to 0.89ng/dl and 2.24 pg/ml. The BUN and creatinine levels were elevated to 45.3 and 2.38 mg/dl, respectively.
Computed tomography showed a 35-mm wide hypervascular tumour close to the main pancreas duct at the pancreas head (Fig. 1). In addition, a 20-mm right adrenal mass and calcification of both the renal pelvis were detected. Ultrasonography of the neck revealed a 13-mm wide adenomatous nodule. Magnetic resonance imaging of the pancreas showed a well-circumscribed nodule, 35 mm in diameter, with high intensity on T2-weighted image.
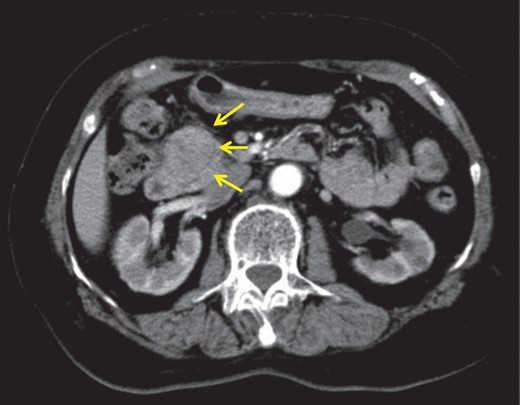
Abdominal enhanced computed tomography revealed hypervascular tumour, 3.5 cm in diameter at the pancreas head.
As a consequence, the patient was diagnosed with insulinoma with MEN1. She underwent palliative treatment of octreotide acetate because surgical treatment was risky for her multiple complications. However, her hypoglycaemia did not improve; thus, she underwent operation after 6 months. The SASI test was not performed because she had renal failure.
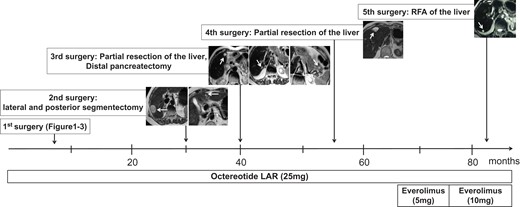
We performed enucleation of the pancreatic head tumour. The postoperative course was good, and she was discharged with normal serum glucose levels. Pathological diagnosis was insulinoma, 3.5 cm, pT2, pN0, pStageII, chromogranin (+), synaptophysin (+), insulin (+), SSTR2A (+), mitoses 3/10 HPF and Ki-67 index: 5% (Figs 2 and 3). Such diagnosis corresponded to NET G2 in the 2010 WHO classification. However, despite undergoing adjuvant treatment of octreotide acetate, multiple metastatic liver lesions were detected after 2 years. Thus, we performed lateral and posterior segmentectomy of the liver. The pathological diagnosis was NET G2, insulin (+), and Ki-67 index: 5%. After 1 year, at 76 years old, she underwent distal pancreatectomy for multiple pancreatic tumours and partial resection of segments 4 and 5 of the liver for metastatic liver tumours. The pathological diagnosis of the pancreatic tumours was NET G1, insulin (−), Ki-67 index: >2%, while that of the liver tumours was metastatic NET G1, insulin (+), and Ki-67 index: <2%. At 77 years old, she underwent partial resection of segment 4 of the liver, which was her fourth surgery. Its pathological diagnosis was metastatic NET G2, insulin (+) and Ki-67 index: 10%. At 80 years old, metastatic liver tumour was detected. However, we performed radiofrequency ablation instead of resection because of her poor performance status and old age. During follow-up, she had continued treatment of Octreotide acetate. Starting at 75 years old, she started taking Everolimus. She survived for 90 months after the first operation (Fig. 4).

Surgical specimen. The tumour was well-circumscribed, white tone, elastic soft.
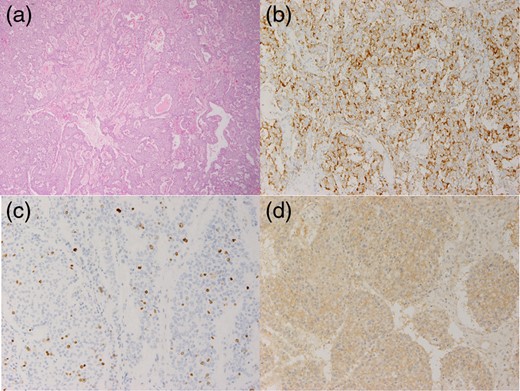
Pathological findings. (a) Hematoxylin and eosin stain (×40): the tumour showed honeycomb arrangement. (b) Insulin staining was positive. (c) Ki-67 index was 5%. (d) SSTR2a staining was positive.
DISCUSSION
MEN1 is classified into two types, namely, familial and sporadic. Familial type is a more common variant that is inherited as an autosomal disorder and is related with a germline MEN1 mutation. Meanwhile, the sporadic type is a less common MEN1 and accounts for approximately only 10% of all MEN1 cases [1]. In our case, the patient did not have familial history of the disease, and we clinically diagnosed her with sporadic MEN1 because she had more than two endocrine tumours: parathyroid tumour, adrenal tumour and insulinoma [2]. Previous studies have reported that insulinoma is usually a benign tumour with low recurrence rate after complete surgical excision [3]. Most insulinomas are NET grade G1 and malignant tumours, with lymph node or liver metastases occurring in only 3.5% of all insulinoma cases [3]. The 5- and 10-year disease-free survival rates are 100 and 96% [3], respectively. In general, insulinoma with MEN1 have higher risk for malignancy than that of insulinoma without MEN1. Some authors reported that 8–27% of insulinoma MEN1 have malignant features [4, 5]. Although it sometimes has a malignant potential, a previous study has reported that 82% of patients with insulinoma with MEN1 achieve hypoglycaemia-free status after the first surgery [4]. The mean age at diagnosis is early at 34.8 years old [6]. Thus, our case was rare because she was old and underwent surgery five times within 7 years.
In recent decades, medical treatment for NETs has been reported to be effective. Octreotide-LAR and Everolimus have been widely applied as primary medical options for insulinomas [7, 8]. Some authors reported the efficacy of a combination of Everolimus plus octreotide-LAR [9, 10]. However, the median progression-free survival was limited to 2 years [7, 8]. Furthermore, our patient had repeated hypoglycaemia, and recurrent tumours were detected every 2 years after surgery despite octreotide-LAR and Everolimus medication. Thus, multimodal therapy, including repeated surgeries, is necessary to achieve long-term survival in patients with NET, particularly those with MEN1 who are prone to have recurrent tumours. Despite the several complications and poor performance status of our patient, she achieved long-term survival because we have selected suitable treatments for her conditions.
CONCLUSIONS
In this report, we discuss about an insulinoma patient with MEN1 who achieved long-term survival via controlled multimodal therapy. We recommend multimodal therapy, including repeated surgeries, for insulinoma patients with multiple complications.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- hypoglycemia
- combined modality therapy
- follow-up
- insulinoma
- karnofsky performance status
- multiple endocrine neoplasia type 1
- neuroendocrine tumors
- octreotide
- pancreatic neoplasms
- pancreaticoduodenectomy
- surgical procedures, operative
- neoplasms
- everolimus
- cellular enucleation
- enucleation procedure
- medical management



