-
PDF
- Split View
-
Views
-
Cite
Cite
Jasdeep Giddie, Rachel Fisher, Andrew White, A rare anatomical variant: transosseous supraclavicular nerve identified during clavicle fracture fixation, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx230, https://doi.org/10.1093/jscr/rjx230
Close - Share Icon Share
Abstract
We describe a rare case of an anatomical variant of the supraclavicular nerve in the intra-operative setting of clavicle fixation for a fracture. Intra-operatively it was noted that one of the supraclavicular nerves was passing through a foramen in the clavicle shaft. A 60-year-old gentleman presented with a displaced multifragmentary fracture of the left clavicle after a fall. Plate fixation with a pre-contoured locking plate was performed under general anaesthesia. The clavicle was exposed through an infraclavicular transverse incision. It was necessary to divide this transosseous nerve branch to permit appropriate plate positioning. Post-operatively the patient was left with some incisional chest numbness. Surgeons should aim to preserve the branches of the supraclavicular nerve although this may not always be possible as we have demonstrated. The patient should be warned about potential deficit.
INTRODUCTION
The supraclavicular nerve is encountered frequently during exposure of the clavicle through a transverse or vertical incision (parallel or perpendicular to the long axis of the clavicle). The likelihood of experiencing post-operative numbness is less using a vertical incision [1]. The frequency of incisional and proximal chest wall numbness ranges from 10 to 29% after operative fixation of the clavicle [2, 3].
The supraclavicular nerve is a superficial sensory branch of the cervical plexus from the nerve roots C3 and C4. The nerve arborizes proximal to the clavicle into the medial, intermediate and lateral branches. It descends under the platsyma and pierces the deep fascia above the clavicle [4]. Nathe et al. [5] dissected out the course of the supraclavicular nerve and its branches and identified that between 2.7 cm from the sternoclavicular joint and 1.9 cm from the acromioclavicular joint, the location of the nerve and its branches is variable and at risk of injury during operative intervention.
A recognized variant of the supraclavicular nerve is a course through the osseous tunnel of the clavicle. This variation is reported in several studies based on post-mortem, surgical and radiological findings with the overall frequency quoted, between 1 and 6.6% [6]. A literature review, identified several articles acknowledging this variant [7–10]. Papadatos et al. [7] concluded that the supraclavicular nerve does not pierce the clavicle but rather is enclosed during the latter ossification stages of the clavicle. In Tubbs et al.’s [8] case report and literature review, he reported that the intermediate branch of the supraclavicular nerve was the most common to be entrapped.
Jelev and Omakawa’s et al. papers [9, 10] are clinically relevant and should make the clinician aware that the supraclavicular nerve entrapment is a differential for shoulder pain. One should recognize in addition to bony entrapment, fibrous and muscular structures may also be implicated as causative factors and lastly the treatment options available include a surgical decompression of the nerve.
We describe the first clinical finding of the transosseous variant in the intra-operative setting of clavicle fixation for fracture.
CASE REPORT
A 60-year-old gentleman presented with a displaced multifragmentary fracture of the left clavicle after a fall from a ladder. After discussion regarding the risks and benefits regarding operative versus non-operative treatment he elected for fixation (Fig. 1).
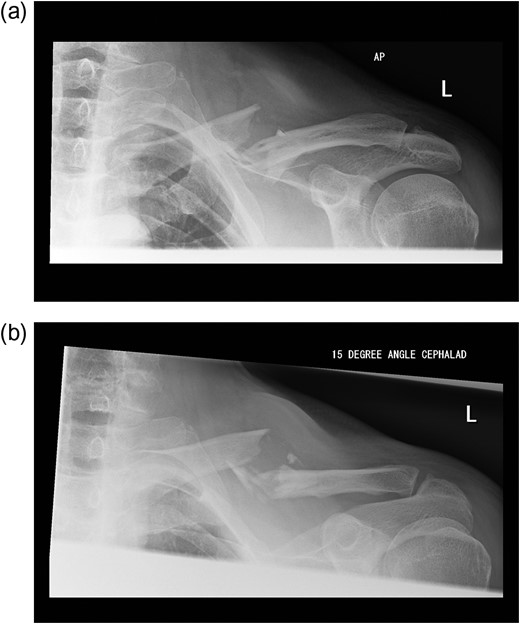
(a and b) Pre-operative radiographs of the fractured clavicle.
Plate fixation with a pre-contoured locking plate was performed under general anaesthesia. The clavicle was exposed through an infraclavicular transverse incision (~1.5 cm inferior to subcutaneous border). The platysma was incised and the supraclavicular nerve branches were identified superficial to the deep fascia. The pectoralis fascia was incised and reflected cranially to expose the superior aspect of the clavicle. It was noted that one of the supraclavicular nerves was passing through a foramen in the clavicle shaft. It was necessary to divide this nerve branch to permit appropriate plate positioning (Fig. 2).
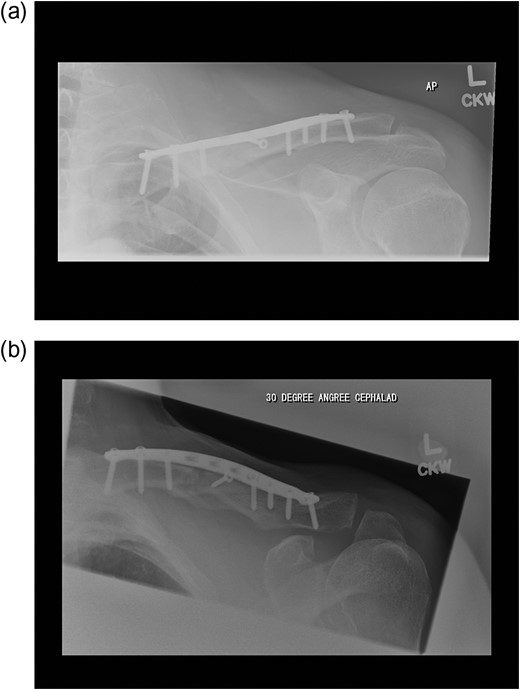
Post-operatively he had some numbness around the surgical incision but experienced no pain. His fracture united by the 12th week (Fig. 3).
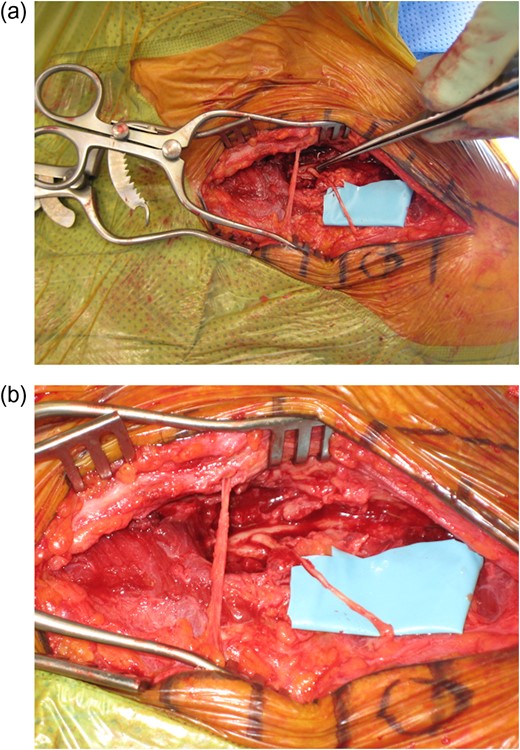
(a and b) Intra-operative pictures demonstrating the intraosseous supraclavicular nerve.
DISCUSSION
With increasing number of clavicle surgeries being undertaken, we are likely to encounter this anatomical variant more often. It can be argued that surgeons should aim to preserve the branches of this nerve to prevent neuroma formation and peri-incisional numbness. This may, however, not always be possible and the patient should be warned about this potential deficit.
CONFLICT OF INTEREST STATEMENT
None declared.



