-
PDF
- Split View
-
Views
-
Cite
Cite
Suha Abdulla, Kathryn Lynes, Sathyan Nagendram, Mansoor Akhtar, Amyand’s hernia managed with open repair and laparoscopic appendicectomy, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx223, https://doi.org/10.1093/jscr/rjx223
Close - Share Icon Share
Abstract
We present a rare case of Amyand’s hernia that was surgically managed using an open repair of hernia combined with laparoscopic appendicectomy. A 68-year-old man presented with an irreducible recurrent right-sided inguinal hernia and abdominal pain. This gentleman had undergone three previous inguinal hernia repairs on the right, and one on the left using the open mesh technique. Ultrasound suggested the possibility of the appendix within the hernial sac and clinical correlation was advised. An open groin approach was taken to repair the incarcerated hernia. This revealed an indirect inguinal hernia containing the appendix with signs of inflammation. The base of the appendix was not visible due to there being a long appendix with fixed cecum in the abdomen. To safely resect the appendix, a laparoscopy was performed and the appendix was successfully removed. The inguinal hernia was repaired using a sutured technique without mesh. There were no post-operative complications.
INTRODUCTION
Amyand’s hernia is defined as the presence of the vermiform appendix within an inguinal hernia sac. It was first described in 1736 by Claudius Amyand who carried out the first recorded appendicectomy, via the inguinal canal, in an 11-year-old boy with a chronically inflamed appendix [1]. This eponymous condition is most commonly identified as an intra-operative finding, and is rare, accounting for around 1% of inguinal hernias presentations [2]. The risk of acute appendicitis within the hernia sac is much lower, ranging from 0.07 to 0.13% [2].
We present a case report on the repair of Amyand’s hernia in which an open groin approach was combined with laparoscopic removal of an inflamed appendix. This is the first combined procedure of its kind described in the UK.
CASE REPORT
A 68-year-old man with a known recurrent right inguinal hernia presented as an emergency with a 1-day history of right iliac fossa pain, and acute irreducibility of the hernia. There were no symptoms indicative of bowel obstruction.
His past medical history included hypertension and chronic obstructive pulmonary disease, and he was taking multiple medications including atenolol, aminophylline and carbocisteine. He was an ex-smoker. His surgical history included recurrent inguinal hernias, with three elective repairs on the right, and one on the left, all using the open mesh technique. His last operation was 20 years ago.
He was apyrexial with no signs of dehydration. Examination of his abdomen revealed a 3 × 3 cm lump in the right groin, which was irreducible and tender to touch.
His full blood count showed a raised white cell count of 14.8 × 109/l, neutrophils of 12.2 × 109/l and CRP of 48 mg/l. Plain abdominal x-ray was unremarkable. Ultrasound confirmed a right-sided inguinal hernia, with the presence of incarcerated bowel. There did not appear to be a loop, and the sonographer suggested that the hernia may contain the appendix; clinical correlation was advised.
At this point, an incarcerated right inguinal hernia with a possibility of appendix or small bowel in the hernial sac was suspected. The patient was prepared for emergency surgery.
An open repair of incarcerated recurrent inguinal hernia was planned with consent obtained for possible laparoscopy or laparotomy. An incision was made in the right inguinal region where long-standing adhesions due to previous surgery were noted. An indirect inguinal hernial sac containing an acutely inflamed appendix was identified (Fig. 1). The base of the appendix was not visible and it was not safe to proceed through the deep inguinal ring. Hence, the appendix was reduced into the abdominal cavity and a laparoscopic repair was deemed suitable.
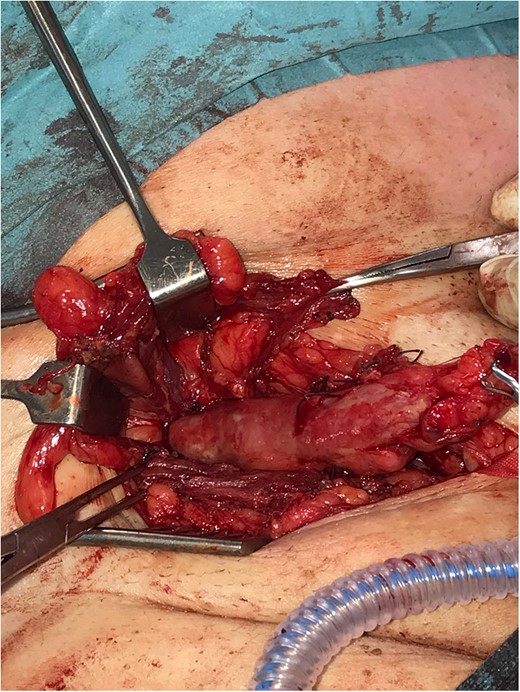
Tip of the appendix within hernial sac identified during open repair.
An open Hasson technique was used to achieve pneumoperitoneum and standard port placement for appendicectomy was used. During laparoscopy the cecum, terminal ileum and appendix were examined. The appendix was grossly inflamed and thickened with a healthy base. There was no evidence of perforation and there was no free fluid or pus present. Laparoscopic appendicectomy was performed and the appendix was removed in an endoscopic retrieval bag.
The hernia repair was then completed with a sutured repair, without mesh, due to the increased risk of infection.
The post-operative period was uneventful. The patient discharged himself from hospital after one day and there were no post-operative complications. The histology confirmed the presence of acute appendicitis; the macroscopic length of appendix was 80 mm.
DISCUSSION
Amyand’s hernia varies widely in its presentation, can occur at any age and typically presents in men [2]. The pathogenesis is unclear and several theories have been proposed. Johnson et al. suggested that appendicitis in such cases could be due to extraluminal compression rather than intraluminal obstruction [3]. The patient in this case had undergone previous mesh repair for a recurrent hernia. It is unclear whether this played any role in the pathology encountered but extensive adhesions were found in the inguinal canal, which may have increased the risk of incarceration. The authors of a previous case of recurrent hernia with appendix mass suggested that scarring around the mesh may have been a factor [4]. Even in non-recurrent cases, incarceration of the appendix is thought to partially result from vulnerability to trauma within the hernia sac, leading to the formation of adhesions [4].
The preoperative diagnosis of Amyand’s hernia is rare. The majority of patients present as an emergency with non-specific signs. In such cases, preoperative imaging would not routinely be used and, therefore, many cases are only identified at the time of surgery. Unusually in this case, due to the recurrent nature of the hernia, preoperative ultrasound was requested and identified the possibility of an Amyand hernia. Preoperative ultrasound diagnosis has previously been reported, but computed tomography scanning is considered the definitive investigation to confirm the diagnosis [5].
Surgery is both diagnostic and therapeutic but there is an ongoing lack of consensus about the optimal operative approach. Three questions remain, firstly is appendicectomy always required? Secondly what approach should be used for this? And finally, what form of hernia repair should be undertaken? In an effort to resolve some of these issues, Losanoff and Basson described a classification system in 2007 as shown in Table 1 [6].
| Types of Amyand hernia . | Features . | Surgical management . |
|---|---|---|
| Type 1 | Normal appendix within the inguinal hernia | Reduction of appendix or appendicectomy and mesh hernioplasty |
| Type 2 | Acute appendicitis with no abdominal sepsis | Appendicectomy through the hernia and sutured hernioplasty |
| Type 3 | Acute appendicitis with abdominal sepsis | Appendicectomy through laparotomy with sutured hernioplasty |
| Type 4 | Acute appendicitis associated with related or unrelated abdominal pathology | Appendicectomy through hernia or laparotomy plus diagnostic workup |
| Types of Amyand hernia . | Features . | Surgical management . |
|---|---|---|
| Type 1 | Normal appendix within the inguinal hernia | Reduction of appendix or appendicectomy and mesh hernioplasty |
| Type 2 | Acute appendicitis with no abdominal sepsis | Appendicectomy through the hernia and sutured hernioplasty |
| Type 3 | Acute appendicitis with abdominal sepsis | Appendicectomy through laparotomy with sutured hernioplasty |
| Type 4 | Acute appendicitis associated with related or unrelated abdominal pathology | Appendicectomy through hernia or laparotomy plus diagnostic workup |
| Types of Amyand hernia . | Features . | Surgical management . |
|---|---|---|
| Type 1 | Normal appendix within the inguinal hernia | Reduction of appendix or appendicectomy and mesh hernioplasty |
| Type 2 | Acute appendicitis with no abdominal sepsis | Appendicectomy through the hernia and sutured hernioplasty |
| Type 3 | Acute appendicitis with abdominal sepsis | Appendicectomy through laparotomy with sutured hernioplasty |
| Type 4 | Acute appendicitis associated with related or unrelated abdominal pathology | Appendicectomy through hernia or laparotomy plus diagnostic workup |
| Types of Amyand hernia . | Features . | Surgical management . |
|---|---|---|
| Type 1 | Normal appendix within the inguinal hernia | Reduction of appendix or appendicectomy and mesh hernioplasty |
| Type 2 | Acute appendicitis with no abdominal sepsis | Appendicectomy through the hernia and sutured hernioplasty |
| Type 3 | Acute appendicitis with abdominal sepsis | Appendicectomy through laparotomy with sutured hernioplasty |
| Type 4 | Acute appendicitis associated with related or unrelated abdominal pathology | Appendicectomy through hernia or laparotomy plus diagnostic workup |
Laparoscopy has been shown to be a useful approach in all forms of incarcerated hernias to assess contents and avoid unnecessary laparotomy. Vermillion et al. first described laparoscopic appendicectomy for a preoperatively diagnosed Amyand hernia in 1999; this was followed by delayed mesh repair of hernia at 1 month [7]. The laparoscopic approach has also been used to facilitate mesh repair by allowing reduction of appendix without opening of the hernial sac [8]. A combined operative approach of sutured open hernia repair with laparoscopic appendicectomy, as used in this case, has been reported and recommended previously [9]. The only previously reported use of laparoscopic appendicectomy in Amyand hernia in the UK was a completely laparoscopic approach used in an 8-week old baby, combined with laparoscopic purse-string closure of hernial orifice [10].
Ultimately, the finding of Amyand’s hernia is so rare that most surgeons would only encounter it once. Decisions are therefore, usually, based on the individual patient and operative features.
CONFLICT OF INTEREST STATEMENT
None declared.



