-
PDF
- Split View
-
Views
-
Cite
Cite
Matthew Rosenzweig, Jessica Marshall, Ronald A White, Misha Tismenetsky, Dwarkanath Shembde, Colo-ovarian fistula, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx228, https://doi.org/10.1093/jscr/rjx228
Close - Share Icon Share
Abstract
Colo-ovarian fistula is a rare entity. The case of a 54-year-old female with a colo-ovarian fistula is presented. We describe our experience in managing this complication of diverticulitis and propose a workup and treatment plan. Initial imaging and diagnostic studies are described. En-bloc resection of the sigmoid colon and ovary was performed. A review of the literature is presented.
INTRODUCTION
There are many documented complications of diverticulitis including, acute phlegmon (22.3%), paracolic abscess (29.5%) obstruction (22.6%), bleeding (4.5%) and perforation (44.5%) [1]. Fistula formation in the setting of diverticular disease is a known complication of the disease process, occurring 10–13% of the time [1, 2]. Typically involving the sigmoid colon, colovesical fistulas occur 65% of the time followed by colovaginal fistulas (25%), coloenteric (6.5%) and colouterine fistulas (3%) [3]. In this case report, we present our experience managing a colo-ovarian fistula in the setting of diverticular disease.
CASE REPORT
A 54-year-old female presented to our colorectal practice after evaluation by her gynecologist with symptoms of abdominal cramps, mucus and bloody vaginal discharge, and recurrent urinary tract infections (UTI). Her only significant surgical history was an IUD removal in 2011. The patient had no significant family history and had not had a colonoscopy. Physical exam revealed the abdomen to be non-tender to palpation with an easily reducible umbilical hernia. She had no rebound tenderness, guarding or palpable masses.
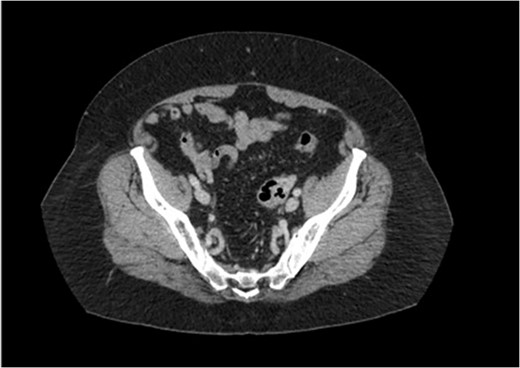
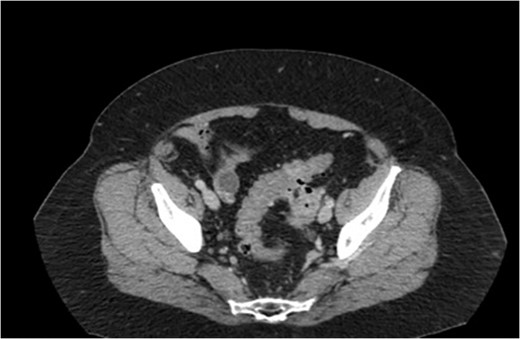
A transvaginal ultrasound, obtained by the patient’s gynecologist, showed a linear hyperechoic structure within the fundal portion of the endometrial canal. The suspicion was that of a retained intrauterine device. In addition, there was a right-sided avascular complex cyst measuring 2.5 × 2.2 × 1.8 cm3. A CT scan of the pelvis was then obtained. The CT scan, highlighted in Figs 1 and 2, revealed multiple foci of gas within the left ovary and fistulization of the adjacent sigmoid colon with questionable air in the fallopian tube.
A colonoscopy was scheduled to exclude a malignancy in the colon and to rule out other colonic pathology. The colonoscopy showed a mild degree of inflammation in the sigmoid colon with diverticular disease and a small amount of purulent exudate. No polyps or tumors were seen.
Two weeks later the patient was taken to the operating room for a hand-assisted laparoscopic colon resection and left oophorectomy. Intraoperatively, there were adhesions between the sigmoid colon and left anterolateral pelvic sidewall. Figure 3 shows the inflamed left ovary and fallopian tube adjacent to the sigmoid colon. The left ovary and a small portion of the left fallopian tube were dissected, and then resected en bloc with the sigmoid colon. Figure 4 depicts the uterus status post-resection. An end-to-end anastomosis was performed to the inraperitoneal rectum. The patient had an uncomplicated hospital course and was discharged home on post-operative Day number 2. One month later, the patient was doing well with normal bowel function, resolution of her UTI’s and resolved abdominal pain.
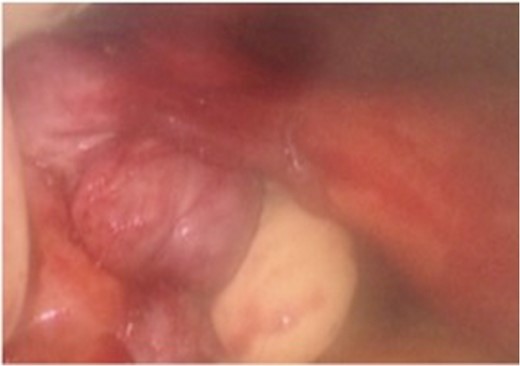
Intra-operative findings of the colo-ovarian fistula including grossly inflamed left ovary and fallopian tube.

Pathologic exam revealed a resected portion of rectosigmoid that contained a diverticulum that had fistulized into the attached ovarian tissue, seen in Fig. 5. An adherent portion of fallopian tube was also present. The fistula tract was lined by granulation tissue with acute and chronic inflammatory cells and focal foreign body giant cells as seen in Fig. 6. The fistula extended into the ovarian stroma, causing a focal tuboovarian abscess. No other diverticula were present.

Gross photograph showing colonic diverticulum extending into pericolonic fat and forming a fistula to the underlying ovarian tissue.
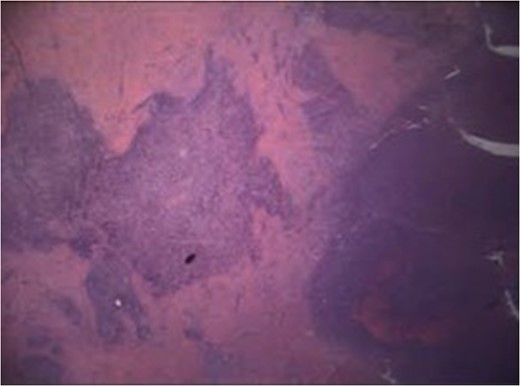
H&E slide, ×20 magnification. Fistula tract (left) lined by granulation tissue and inflammatory cells extending into ovarian stroma (right).
DISCUSSION
Fistulas between the colon and ovary have rarely been reported. Of those involving the genital tract, colovaginal and colouterine fistulas are reported most often while salpingo-enteric and colo-ovarian fistulas are reported least often [4–6].
Common causes for a colonic fistula include pelvic inflammatory disease, appendicitis, Crohn’s disease and diverticulitis. Extension of localized inflammation is the most likely etiology. With diverticular perforation or rupture, inflammation can lead to adhesion formation and the associated inflammatory response can lead to the creation of a fistula [7–10]. Symptoms may initially reflect the underlying disorder before features of a fistula present [9]. Eventually, symptoms of a colo-ovarian fistula may include lower abdominal pain, low-grade fever, malaise, palpable masses in the pelvis, UTI and vaginal discharge.
As the condition is rare, there is no evidence-based algorithm for imaging a suspected colo-ovarian fistula. After a literature review, it is our opinion that there is not sufficient evidence to suggest the best pre-operative diagnostic imaging modality to diagnose an internal diverticular fistula. Combinations of pelvic ultrasound, CT scan, colonoscopy or barium enema have been used successfully for diagnosis and perioperative planning [5, 6, 9]. Operative management of internal fistulas has varied. Resection with primary anastomosis is the procedure of choice. Resections with primary anastomosis followed by prophylactic diversions, Hartmann procedure and three-stage procedures have all been described [3, 9]. In our case, the patient was safely treated with a single procedure that allowed for en-bloc resection of the sigmoid colon and ovarian fistula. The laparoscopic approach allowed for a quicker recovery period.
Colo-ovarian fistula is a rare entity with only a few reported cases. The authors present their experience and discuss their workup and management. While there is no established consensus on the workup and treatment of colo-ovarian fistulas, we present a successful approach.
CONFLICT OF INTEREST STATEMENT
None declared.



