-
PDF
- Split View
-
Views
-
Cite
Cite
Emmanuel Katsogridakis, Goran Pokusevski, Peter Byrne, Acute appendicitis presenting as a complicated inguinal hernia: a case of left-sided Amyand’s hernia in an elderly man, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx224, https://doi.org/10.1093/jscr/rjx224
Close - Share Icon Share
Abstract
Amyand’s hernia (AH) is characterized by the presence of the vermiform appendix in an inguinal hernia sac. Typically presenting on the right side and with manifestations similar to those seen in complicated hernias, it presents a diagnostic challenge and is frequently only diagnosed intraoperatively. We present the case of a left-sided AH on a 75-year-old man treated with appendicectomy, orchidectomy and hernioplasty without mesh.
INTRODUCTION
Amyand’s hernia (AH) is a type of inguinal hernia characterized by the presence of the vermiform appendix (VA) in the hernia sac. It is rare clinical entity comprising ~1% of all inguinal hernias and therefore when symptomatic, presents a diagnostic dilemma [1, 2]. Unsurprisingly, the diagnosis may only be established intraoperatively in significant number of cases.
Typically AHs are encountered on the right side, however, a small number of left-sided cases have also been reported and are considered to be associated with situs inversus, a mobile caecum or intestinal malrotation [3].
We present a case of a left-sided AH on a 75-year-old man presenting as a complicated inguinal hernia, which was managed with an appendicectomy, inguinal orchidectomy and no-mesh hernioplasty.
CASE REPORT
A 75-year-old gentleman presented as an emergency admission with a 3- day history of a painful and irreducible left inguinal hernia. Though the symptoms had progressively worsened over the course of those 3 days, the history and symptoms were not suggestive of bowel obstruction. His past medical history was significant for advanced dementia due to Alzheimer’s disease, rheumatoid arthritis and hypertension. The left-sided inguinal hernia for which he presented on this admission had first appeared 6 months prior to this episode and had to this point been asymptomatic.
Physical examination revealed a large left inguinal lump that was tender and irreducible, without associated skin changes suggestive of an incarcerated inguinal hernia. Routine preoperative work-up revealed a C-reactive protein of 103 mg/l but was otherwise unremarkable. Due to the patient's lack of capacity to provide informed consent, a discussion was had with his next of kin who also held legal power of attorney. A decision was made to proceed with an open repair of this suspected incarcerated inguinal hernia.
Through a left groin incision, the inguinal canal was opened and a thickened cord with signs of chronic inflammation was seen and mobilized. The sac was dissected free and opened, and its content inspected, revealing the presence of the caecum and of an inflamed appendix with a gangrenous tip (Fig. 1). An appendicectomy was performed and the sac was closed and reduced into the abdominal cavity in the standard fashion. At this stage, it was considered prudent to proceed with a hernioplasty without mesh. To facilitate a more robust sutured repair, we proceeded with a left-sided orchidectomy and a suture two-layer repair.
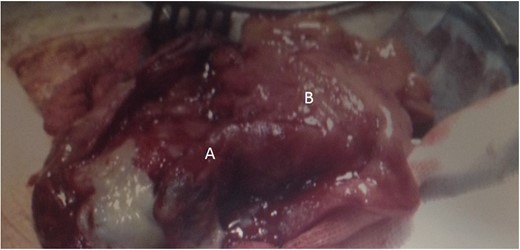
Left-sided inguinal hernia containing the VA (A) and caecum (B). Note the inflammatory changes and the gangrenous tip consistent with appendicitis.
The patient had an uneventful post-operative course and was discharged the following day. On further follow up, he continues to remain completely free of symptoms.
DISCUSSION
AH is a rare clinical entity that comprises <1% of all inguinal hernias [4]. Though the majority of cases is right-sided, cases affecting the left side have also been reported, and are associated with situs inversus, a mobile caecum and intestinal malrotation [3]. There is a paucity of data in the literature regarding the exact incidence of left-sided AHs. However in a large paediatric series reported by Cigsar et al. [5] only 2 out of 46 cases were seen on the left side (n = 2/46 or 4.3%). Interestingly, both cases were asymptomatic. In a review of the paediatric surgical literature, Al-Mayoof et al. [4] identified and reported on 10 cases of left AH between 1998 and 2013.
The clinical presentation of AH varies significantly and can range from asymptomatic cases, particularly in the paediatric population, to symptoms and signs mimicking a complicated inguinal hernia. Rarely, they may also present as scrotal abscesses or with symptoms of acute scrotum [6–8]. Establishing an accurate and timely diagnosis therefore remains a challenge, and a high index of clinical suspicion is required.
Computed tomography (CT) and ultrasonography have been shown to aid in establishing an accurate diagnosis when AH is suspected [9]. The role of preoperative imaging however remains controversial for two main reasons. On the one hand, the diagnosis is frequently established intraoperatively, as the patient has been managed for suspected strangulated or incarcerated hernia, a setting in which further imaging investigations are not frequently undertaken. On the other, this condition is frequently prevalent in the paediatric population, where the risks of ionizing radiation of CT may outweigh the benefits, while ultrasound frequently is unable to elucidate the diagnosis due to the presence of the air-filled caecum [5].
The treatment of AH remains the subject of an ongoing debate, particularly with regards to whether an appendicectomy is required in cases with a grossly normal VA and also regarding the use of mesh. Despite a recent communication in which four subtypes of clinical manifestation of AH were identified and a treatment algorithm was promulgated for each one, there is a lack of consensus regarding the optimal surgical management of these patients [10].
The advocates of performing an appendicectomy in every case argue that it prevents future morbidity from appendicitis and also the possibility that intraoperative handling of the VA may potentially lead to appendicitis in the future. The opponents of this approach cite the important role of the VA in paediatric surgical procedures, its immune role in the paediatric population and the rather low incidence of concomitant appendicitis in patients with AH, which is <0.1% [4, 5–7]. Thus, a case by case approach is advised.
In our case, the patient’s symptoms were due to acute gangrenous appendicitis. Though the exact association of AH with developing appendicitis is poorly understood, it is believed to be secondary to a reduction in blood flow resulting from either adhesions that make the hernia irreducible or to extrinsic compression onto the appendicular vasculature by the external inguinal ring. As the appendix was gangrenous, the need for performing an appendicectomy and avoiding a mesh repair of the hernia was unequivocal.
CONCLUSION
Left-sided AH is a rare clinical entity that requires a high index of clinical suspicion and is most commonly diagnosed intraoperatively. There is a lack of consensus in the literature regarding the optimal management of patients with grossly normal vermiform appendices, and a case by case consideration is advised, particularly in the paediatric population, due to the low incidence of appendicitis in AH.
CONFLICT OF INTEREST STATEMENT
None declared.



