-
PDF
- Split View
-
Views
-
Cite
Cite
Erion Qaja, Carol Le, Ramon Benedicto, Repair of giant inguinoscrotal hernia with loss of domain, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx221, https://doi.org/10.1093/jscr/rjx221
Close - Share Icon Share
Abstract
A massive inguinoscrotal hernia extending below the midpoint of the inner thigh, in a standing position, constitute a ‘giant’ inguinoscrotal hernia. A 74-year-old male presented with giant left sided inguinal hernia for the last 30 years. Patient underwent open repair under general anesthesia after perioperative respiratory exercise. Standard hernia repair identified a sliding hernia containing entire omentum, small and large bowel, and the appendix. Giant hernias pose a challenging problem because reduction of the hernia contents inside the abdominal cavity may increase intra-abdominal and thoracic pressures. Recurrence remains an issue for these patients after successful meshoplasty and debulking of abdominal contents. We describe a simple reduction with biological mesh repair, omentectomy, small bowel resection and sigmoidopexy as a viable technique for patients with greater than 50% of abdominal contents in the inguinoscrotal region with complete loss of domain.
CASE REPORT
A 74- year-old male presented with a history of progressively increasing irreducible left inguinal with left scrotal swelling for 30 years. He had no history of difficulty in voiding and constipation. He had a systolic CHF, as evidenced by a recent cardiac catheterization. He is a previous smoker. On examination, he had left inguinal swelling and massive scrotal swelling Fig. 1 reaching the level of the midthigh. In addition, he had dilated veins over the scrotum and bowel peristalsing on the left scrotum.

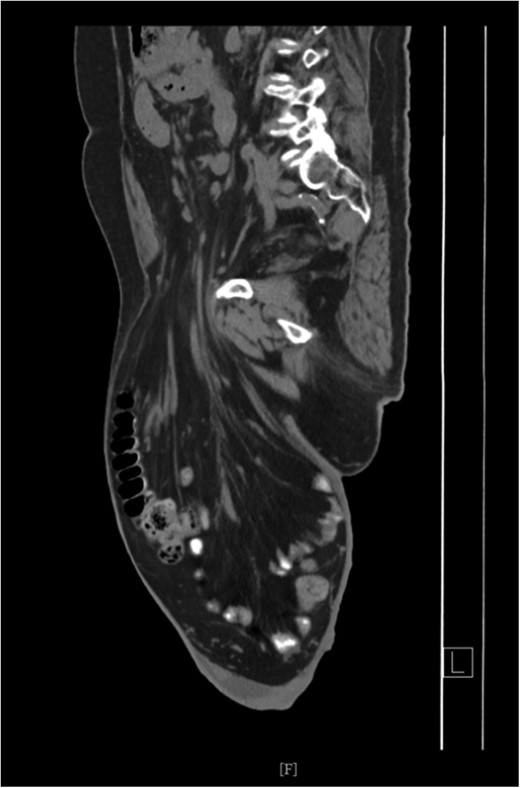
Pulmonary function test revealed no abnormalities. Electrocardiogram was normal, however, an echocardiogram confirmed systolic congestive heart failure with an ejection fraction of 30%. Patient preoperatively underwent a rigorous respiratory exercise and cardiac evaluation. Pre-operative computed tomography (CT) scan showed omentum, small and large bowel within the left scrotum Figs 2 and 3. Consent for the procedure was obtained including orchiectomy, bowel resection. Patient was mechanically bowel prepared the night prior to surgical intervention.

CT Scan showing small and large bowel within left scrotal sac.
DISCUSSION
Giant hernias are usually the results of neglect and fear of surgical procedure. They are common in rural populations. Patients would typically present with voiding difficulty. Pressure wounds are common in the medial aspect of the thigh as well as the scrotum. As shown on pre-operative pictures, the penis is buried inside the scrotum. The social impact is significant, which can cause social isolation, a fear of seeking medical attention, and subsequently, a worsening of the condition [1]. Although, the defect is usually large, small bowel obstruction and strangulation has been described. Contents of the hernia vary, but the small and large bowel, the bladder, the ovaries and, occasionally, the stomach have been reported [2].
The chronic nature of the disease poses a challenge to the patient post-operatively, as the reduction of the hernia contents back to the abdominal cavity can lead to an abrupt increase in intra-abdominal pressure, a reduction of venous return, and a decrease excursion of the diaphragm. A reduction in tidal volume, a post-operative ileus and a risk of intra-abdominal compartment syndrome are potential post-operative complications in the immediate post-operative period. Elective mechanical ventilation, peak airway pressure monitoring, bladder pressure measurement and frequent abdominal examination should all be part of post-operative management [3, 4].
Recurrence is significantly higher in giant hernias. Tension-free repair can reduce the rate of recurrence. Drains can be placed to avoid the risk of hematomas; however, in our case, we avoided placing drains because of the possibility of mesh infection. Scrotal skin, although post-operatively redundant, generally should be left intact because of contraction of the dartos muscle. Additionally, should patient require abdominal decompression because of an increase in intra-abdominal pressures, then the abdominal contents can be reduced back to the scrotum, where the scrotum functions as an ‘anatomical silo [5].’
Intraoperatively a classic hernia incision was made over the left inguinal ligament. The sac was mobilized around the scrotal area and was eventually opened. Reducing the hernia contents proved to be impossible, thus a debulking omentectomy was performed. Small bowel was reduced first, followed by the descending and transverse colon; a portion of sigmoid colon was reduced last. We avoided resecting any portion of the bowel; this gave us the flexibility to use a biological Phasic Mesh to cover the floor in a modified Lichtestein technique Figs 4 and 5. Patient was extubated on post-operative Day 1, and subsequently discharged on post-operative Day 4.

Reduction of left hernia contents within abdominal cavity. Note significant distension of the abdomen in this post-operative photograph.

Redundant skin in the left scrotum left purposely intact should patient require decompression of abdominal contents due to increase of intra-abdominal pressure.
CONCLUSION
Giant inguinoscrotal hernias are rare. Patients undergoing elective herniorrhaphy should undergo extensive pre-operative evaluation including pulmonary and cardiorespiratory risk stratification. Physicians should be aware of the post-operative complications in order to reduce the incidence of cardiorespiratory problems, wound complications, and recurrence rates.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT
Patient has provided written consent in regards to publication of the manuscript as well as any pictures associated with it.



