-
PDF
- Split View
-
Views
-
Cite
Cite
Krish Kulendran, Cian Keogh, Heng-Chin Chiam, Laparoscopic repair of a right diaphragmatic hernia in a post-partum lady, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx194, https://doi.org/10.1093/jscr/rjx194
Close - Share Icon Share
Abstract
Traumatic diaphragmatic injuries (TDI) are often challenging to diagnose. Research suggests that no single diagnostic study is sensitive or specific enough to identify such an injury, unless there is established herniation of intrabdominal contents. It is a rare cause of small bowel obstruction, which carries a substantial mortality rate. This report describes a case of a 41-year-old pregnant female who presented with irretractable vomiting and abdominal pain secondary to a delayed presentation of right-sided TDI. The most accepted mechanism regarding TDI is due to sudden elevation in the pleuroperitoneal pressure gradient. This case is unusual given its mechanism of injury during pregnancy and its right-sided location. She underwent laparoscopy which facilitated successful reduction of the hernial and closure of the defect. Postoperatively, she made an excellent recovery and was discharged within a few days. This report aims to increase the awareness amongst surgeons.
INTRODUCTION
In 1579, Pare described two patients who died of strangulated intra-abdominal organs through diaphragmatic defects [1]. Presentations of traumatic diaphragmatic injuries (TDI) continue to be clinically challenging to identify given their occult features. Though incredibly uncommon, timely diagnosis is critical given its mortality rate of 31%; with increasingly morbid consequences in pregnancy [2]. TDI are associated with 6% of all major thoracic injuries [2]. This case details a post-partum woman with a right-sided TDI.
CASE REPORT
A healthy 41-year-old female, 38-week pregnant, presented with irretractable abdominal pain and vomiting. There was no previous similar history or abdominal surgery. She associated the onset of symptoms with a low energy fall on to her buttocks. There was no improvement despite hastening her elective caesarean section. Thereafter, she was treated as a post-operative ileus (Fig. 1). On multiple examinations, she remained afebrile and haemodynamically stable. The abdomen was distended, with generalized mild tenderness. Bowel sounds were audible. Blood tests were unremarkable. Failure to progress prompted further evaluation with CT. This revealed a small bowel obstruction secondary to a right-sided diaphragmatic hernia (Fig. 2). After resuscitation, she proceeded to laparoscopy.


A 10 mm port was inserted infraumbilically using Hasson technique, with an additional three operating ports. Laparoscopy confirmed radiological findings of a right-sided diaphragmatic defect with herniation of terminal ileum.
There was evidence of small bowel obstruction, with distended small bowel loops and constriction at the defect. The defect’s location did not appear consistent with a congenital hernia. The hernia was reduced by gentle traction and the defect was closed laparoscopically with interrupted 0-monosof sutures. The entire small bowel was viable and intact (Fig. 3).
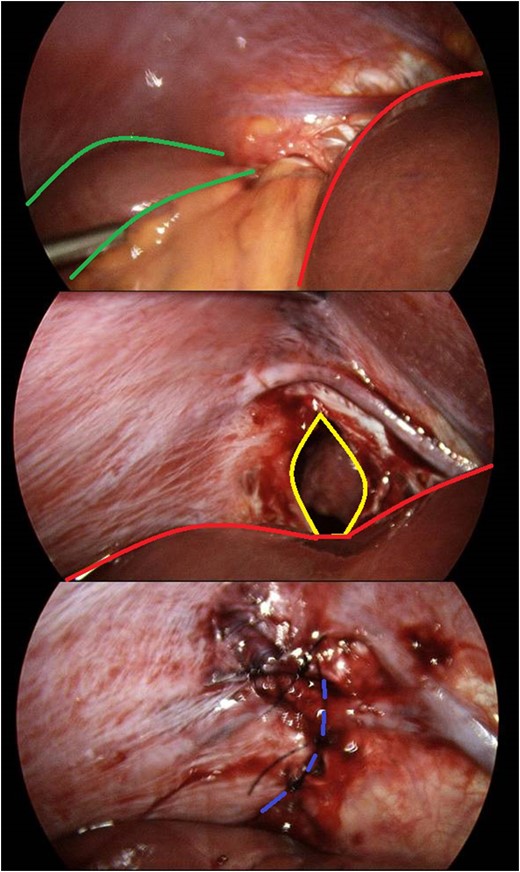
Identification and laparoscopic reduction of diaphragmatic hernia in sequence. Green borders outline small bowel; red borders delineates hepatic edge; yellow margins signifies diaphragmatic defect; and purple hashed line is closed defect.
The recovery was uncomplicated and the patient was discharged home 2 days postoperatively.
DISCUSSION
This is an unusual case of a right-sided TDI. They are commonly caused by high energy blunt thoracoabdominal trauma, and are more common on the left side [1, 2]. The intrathoracic negative pressure draws in intra-abdominal contents [1].
The most accepted mechanism for TDI involves sudden elevation in the pleuroperitoneal pressure gradient [3]. The left hemidiaphragm has a congenital weakness along the embryonic lines of fusion, which predisposes it to TDI in blunt trauma [1–3]. The right hemidiaphragm by contrast has the liver, along with its diaphragmatic attachments, as a protective presence. This accounts for a significantly lower incidence of right transdiaphramatic herniation [1–3].
Due to greater forces required for right-sided TDI, there is an associated higher pre-hospital mortality rate when compared with left. This is due to associated severe hepatic or vascular injuries [3].
Diligence is prioritized to lethal injuries during an emergency operation. Examination for a diaphragmatic hernia should be incorporated into a thorough trauma laparotomy.
TDI is often challenging to diagnose. Research has shown that no single diagnostic study is sensitive or specific enough to identify an acute diaphragmatic injury unless there is established herniation of intrabdominal contents [1, 3].
This case was further complicated by a recent operation and thus initially managed as an ileus. Her clinical picture may have warranted a CT scan immediately post delivery of foetus.
A systematic review performed by Lu et al, revealed rates of missed TDI were as high as 66% [3]. It can present months to years after injury with incarcerated abdominal viscus or respiratory compromise owing to reduced intrathoracic volume [3]. It is clear that missed TDI, portends a poorer prognosis.
Minimally invasive procedures such as laparoscopy or thoracoscopy can be utilized to diagnose and treat TDI for if there is a suspicion. A number of methods have been described when closing the diaphragmatic defect. These include interrupted sutures, prosthetic mesh or even a peduncled flap using the falciform ligament [1, 3].
Diaphragmatic hernias must be diagnosed and repaired before onset of labour due to their life threatening complications [4]. High pressure exerted by a growing uterus throughout pregnancy coupled with diaphragmatic contraction and bearing down during labour, force the abdominal viscera into, and cause enlargement of diaphragmatic defect [4].
This case highlights the rarity, diverse features and diagnostic dilemmas associated with delayed TDI presentations. Thankfully in this case there were no complications. The mechanism of injury described in this case is unusual for blunt trauma TDI. The energy in combination with her advanced pregnancy may explain it, and serves as a reminder to clinicians to maintain vigilance.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLOSURE STATEMENT
Informed consent was obtained from the patient for publication of this case report and accompanying images. Approval was also granted from the ethics committee. There were no potential conflicts of interest in generating this report. Nil financial support or sponsorship was obtained for this article. This article is not been previously published or under any consideration elsewhere.



