-
PDF
- Split View
-
Views
-
Cite
Cite
Shreesh Kolekar, Tejas Chincholi, Ashok Kshirsagar, Ritvij Patankar, Giant splenic hemangioma in a 10-year-old boy treated with a spleen saving surgery, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx217, https://doi.org/10.1093/jscr/rjx217
Close - Share Icon Share
Abstract
Tumors of spleen are rare. The most common benign tumor of spleen is hemangioma. Most splenic hemangiomas (SH) tend to be discovered in mid-30s to mid-50s. SH are discovered incidentally in most of the cases as they are usually asymptomatic. Small asymptomatic SH can be managed with observation. The treatment options for large hemangiomas are embolization of the splenic arterial branch, splenectomy by laparotomy or laparoscopy. Partial splenectomy can be done if the lesion is small and located at the poles of the spleen. We present a rare case of splenic hemangioma in a 10-year-old boy who presented with a painless palpable mass in the left upper abdomen. On CT scan—A large well-defined cystic lesion with few thin enhancing septa within it is seen involving the spleen. Laparotomy was done followed by Partial splenectomy. The histopathology report was suggestive of Cavernous Hemangioma of spleen.
INTRODUCTION
Hemangiomas are the most common benign primary neoplasm of spleen, yet they remain as a rare disorder. Less than 100 cases have been reported so far. The average age of presentation is 63 years. Most of the patients are asymptomatic, rest of the patients presenting with pain and a lump in the abdomen. Majority of the splenic hemangiomas (SH) remain small in size rarely reaching a large size. Small hemangiomas can be observed safely but large, symptomatic hemangiomas can be treated by splenectomy.
CASE REPORT
A 10-year-old boy was brought to the hospital by the parents with the complaint of a painless lump in the left upper abdomen which they noticed a week ago. Patient was afebrile. Physical examination revealed splenomegaly extending 4 cm below the coastal margin, which was non-tender, rest of the examination was normal. No other clinical signs were detected.
Hemoglobin, leucocyte and platelet counts were normal. Ultrasonography revealed a large hypoechoic cystic lesion involving the spleen measuring 108 × 98 mm with thin internal septa. CT scan—A large well-defined cystic lesion with few thin enhancing septa within it is seen involving the spleen. The lesion is causing mass effect and displacing adjacent vessels and bowel loops (Figs 1, 2).
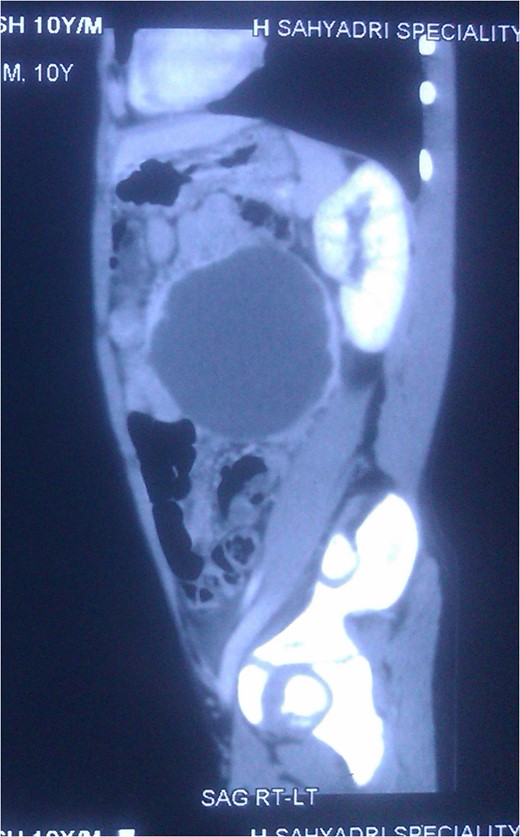
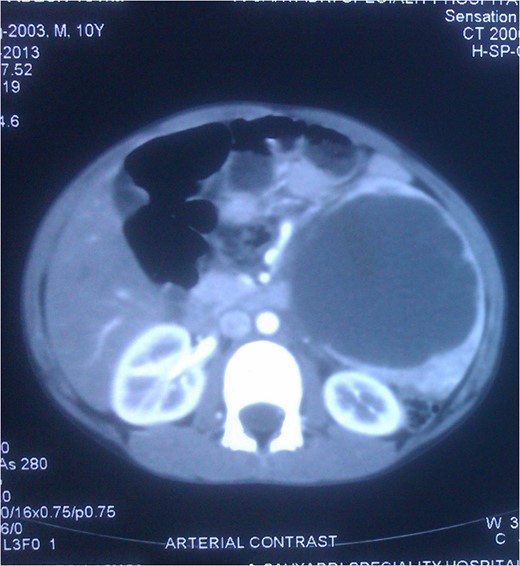
CT Scan: Cross section showing the splenic mass almost reaching the midline.
The patient underwent laparotomy, during which, the spleen was enlarged measuring approximately 11 cm × 10 cm × 5 cm with the cystic lesion involving the lower pole (Fig. 3). The fluid in the splenic cyst was aspirated, which was brownish in colour. Partial splenectomy was done. The histopathological report revealed—true congenital splenic cyst with cavernous hemangioma. Post-operative period was uneventful.
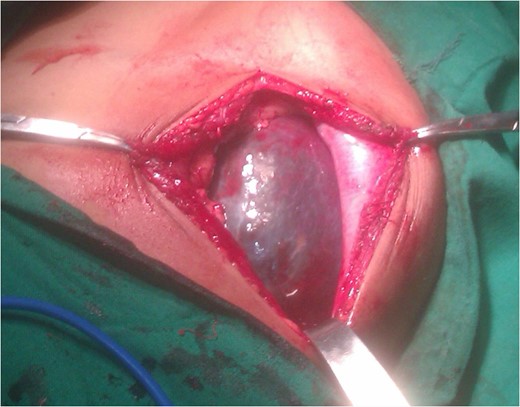
Intraoperative photo of the splenic mass showing the cystic lesion.
DISCUSSION
Cysts and tumors of the spleen are uncommonly encountered in clinical practice. The most common type of splenic cystic neoplasm is hemangioma. The angiomas are considered congenital, as they are usually present at birth [1]. Less than 100 cases have been reported in the English literature. Splenic cysts although noted in all age groups, are most common in the second and third decade of life. In most of the cases they are incidental radiological, surgical or autopsy findings. In spite hemangioma being reported as benign, the potential for angiosarcoma is known, especially when the size of the spleen is big.
A hemangioma is a slow growing neoplasm consisting of an overgrowth of new blood vessels. SH can be single, multiple or involving the entire organ. An asymptomatic abdominal mass is the presenting feature in 30–45% of cases. Splenomegaly, abdominal pain, dyspnea, diarrhea or constipation can be the presenting feature in few cases. A hematologic clue to the existence of splenic hemangioma may present as unexplained consumptive coagulopathy caused by platelet trapping. In children, abdominal symptoms such as pain and physical examination findings are present when cysts are larger than 8 cm [2]. There is significant variation in the age of presentation splenic hemangioma with an average age of presentation/detection of between 51 and 63 years [3]. There is no predilection towards any race or gender.
SH appear as round, hypo, iso or hyper echogenic masses on ultrasound, based on their exact composition. Unenhanced CT scans can show a low-attenuation mass; following IV contrast, the vascular channels show centripetal fill (from the periphery inward). Larger lesions can fill more slowly and may do so incompletely and inhomogeneously. They may contain calcifications and may show peripheral enhancement after intravenous contrast injection. The size of the tumour removed because of the symptoms is much larger than those which are found incidentally at the surgery or autopsy. Grossly, SH may present in a wide variety ranging from cystic to solid. Microscopically, SH may be capillary or the more common cavernous type. The usual picture is that of vascular spaces lined by a single layer of bland endothelial cells, without mitoses.
The complications that may occur because of SH are spontaneous rupture, with haemorrhage, is a risk with larger lesion. Some patients may present with Kasabach-Merritt syndrome. Thrombosis and infarction can also occur because of the abnormalities in the vascular supply of the tumour.
The natural course of SH is very slow growth over time. The treatment options ranges from regular follow-up to total splenectomy, depending on whether the tumour is symptomatic or asymptomatic and also on the size of the tumour. When the tumour is small and asymptomatic, only regular follow-up is needed. Partial splenectomy can be done when the tumour is symptomatic and is at one of the poles. Total splenectomy can be done when the tumour is massive in size or laparoscopic splenectomy is planned. Other treatment modalities which can be helpful are embolization of the specific splenic arterial branch to the SH with or without anti-angiogenic agents, which are based on the age of the patient and the site and size of the lesion [4].
CONFLICT OF INTEREST STATEMENT
None declared.



