-
PDF
- Split View
-
Views
-
Cite
Cite
Masatsugu Hiraki, Junji Ueda, Hiroshi Kono, Noriyuki Egawa, Kiyoshi Saeki, Yasuhiro Tsuru, Takao Ide, Hirokazu Noshiro, A case of Mirizzi syndrome that was successfully treated by laparoscopic choledochoplasty using a gallbladder patch, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx212, https://doi.org/10.1093/jscr/rjx212
Close - Share Icon Share
Abstract
The use of laparoscopic surgery in the treatment of Mirizzi syndrome is considered controversial due to the degree of technical difficulty. We herein describe the case of a 36-year-old woman who was admitted to our hospital due to appetite loss, nausea and back pain. Endoscopic retrograde cholangiography revealed a round-shaped filling defect at the confluence of the bile duct. The patient was diagnosed with Mirizzi syndrome Type II according to the Csendes classification. Before surgery, an endoscopic nasobiliary drainage tube was placed for intraoperative cholangiography. Based on the intraoperative findings, the anterior wall of Hartmann’s pouch was excised to remove the impacted gallstone. The neck portion of the gallbladder wall was then used to make a gallbladder patch, which was sutured to cover the anterior wall of the common hepatic bile duct. Laparoscopic choledochoplasty using a gallbladder patch was a technically feasible treatment for Mirizzi syndrome Type II.
INTRODUCTION
Mirizzi syndrome is an unusual complication of cholecystolithiasis that is characterized by the obstruction of the common hepatic duct due to the impaction of a gallbladder stone in the cystic duct or the neck of the gallbladder [1]. In addition, Mirizzi syndrome is sometimes associated with cholecystocholedochal fistula. In such patients, a non-circumferential defect of the choledochus is observed after the extraction of the gallbladder. The choledochus must be repaired appropriately, using methods such as direct suturing or choledochoplasty. However, laparoscopic choledochoplasty may be considered challenging due to the technical difficulty.
CASE REPORT
A 36-year-old woman was admitted to our hospital due to appetite loss, nausea, and back pain. A physical examination disclosed right hypochondriac tenderness and obvious jaundice. Laboratory studies showed elevated levels of total bilirubin (9.7 mg/dl), direct reacting bilirubin (6.0 mg/dl), aminotransferase (AST 281 U/l, ALT 362 U/l), alkaline phosphatase (1945 U/l,) and γ-glutamyltransferase (1769 U/l); however, her white blood cell count and C-reactive protein level were within the normal ranges. Magnetic resonance cholangiography revealed that the intrahepatic and common hepatic bile ducts were dilated, and that the gallbladder was distended (Fig. 1). Endoscopic retrograde cholangiography demonstrated a round-shaped filling defect at the confluence of the bile duct (Fig. 2). Based on the findings, the patient was diagnosed with Mirizzi syndrome Type II according to the Csendes classification [1]. Although, the endoscopic removal of the impacted gallstone was unsuccessful, a stent tube was placed for endoscopic retrograde biliary drainage in order to improve the patient’s obstructive jaundice. We planned to perform laparoscopic surgery.
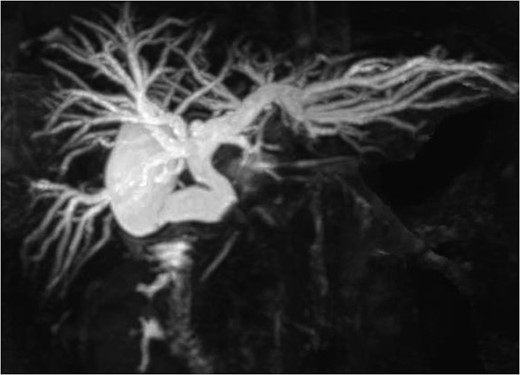
Magnetic resonance cholangiography showed the dilated intrahepatic biliary tree, the common hepatic duct and the gallbladder.
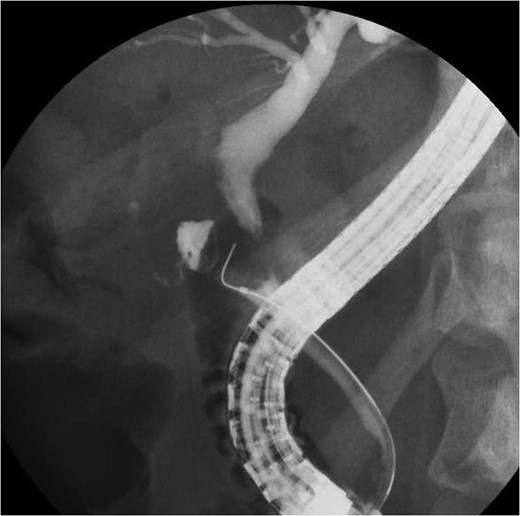
Endoscopic retrograde cholangiography demonstrated a filling defect at the confluence of the bile duct.
Before surgery, the stent tube was changed to an endoscopic nasobiliary drainage (ENBD) tube for intraoperative cholangiography. The initial intraoperative examination revealed the marked thickening of the gallbladder wall. First, the anterior wall of Hartmann’s pouch was excised to remove the impacted gallstone (Fig. 3). After the removal of the gallstone, a cholecystocholedochal fistula was identified. The gallbladder was then excised and the remaining neck portion was used to perform choledochoplasty using a gallbladder patch. The gallbladder patch was sutured to cover the anterior wall of the common hepatic bile duct (Fig. 4). Intraoperative cholangiography was performed to confirm the absence of bile leakage and bile duct stenosis.

The intraoperative findings: The anterior wall of the cystic duct and the common hepatic duct was dissected to remove the gallstone.

The intraoperative findings: The gallbladder patch was sutured to the dilated cystic duct and intraoperative cholangiography was performed.
The postoperative course was uneventful. The patient was discharged from hospital on the 5th day after surgery. Magnetic resonance imaging at 6 months after surgery revealed the good passage of the bile duct.
DISCUSSION
Mirizzi syndrome is defined as extrinsic compression of the common hepatic duct by an impacted stone in the cystic duct or the gallbladder neck [1]. Our case was classified as Mirizzi syndrome Type II (according to the Csendes classification [1]), based on the presence of a cholecystocholedochal fistula, the diameter of which was one-third of the circumference of the common hepatic duct. The incidence of Mirizzi syndrome among patients with gallstones is reported to range from 0.63 to 5.7% [2–4]; 15–57% [4, 5] of these patients are reported to have Mirizzi syndrome Type II.
Subtotal cholecystectomy, in which a minimal portion of the neck side of the gallbladder is left in place, is considered to be the best treatment for Mirizzi syndrome Type I [5]. In Mirizzi syndrome type IV, hepaticojejunostomy with the Roux-en Y method is preferred due to the extensive destruction of the bile duct wall [5]. In Types II and III, direct closure and patch repair using the gallbladder or cystic duct should be considered in order to restore the biliary passage [1, 5]. In our case, although the excision of the anterior wall of Hartmann’s pouch to extract the impacted gallstone was minimized, the excision reached the common hepatic duct. After the extraction of the impacted gallstone, the nasobiliary tube that had been placed in the bile duct was easily identified. Thus, choledochoplasty was performed using a gallbladder patch rather than direct closure in order to preserve the biliary passage. Several reports have suggested that choledochoplasty using a gallbladder patch is useful [1, 5]. However, few reports have described performing this operation by a purely laparoscopic approach. Kumar et al. [4] investigated 169 Mirizzi syndrome patients who were treated with surgery. In that report, 146 (86%) patients were treated with open surgery. Laparoscopic surgery was attempted in the remaining 23 (14%) cases, but was only successful in one case involving a patient with Mirizzi syndrome Type II. Antoniou et al. [6] reported that laparoscopic treatment was successfully applied in 59% of Mirizzi syndrome cases.
The use of laparoscopic surgery in the treatment of Mirizzi syndrome is considered to be controversial due to the technical difficulty [7]. Laparoscopic surgery for Mirizzi syndrome is reported to be associated with a high risk of conversion to open surgery (41%), complications (16%) and reoperation (5%) [6]. However, in recent years, laparoscopic surgery has steadily progressed and advanced techniques have been applied in the treatment of various types of disease [8]. Laparoscopic subtotal cholecystectomy, with the extraction of impacted stones has been reported to be successful in cases of Mirizzi syndrome [4, 6, 9]. However, choledochoplasty is often required in order to restore the biliary passage in patients with Mirizzi syndrome Type II [1, 5]. Thus, laparoscopic choledochoplasty may be a treatment option for Mirizzi syndrome Type II.
The insertion of an ENBD tube is recommended prior to laparoscopic surgery for Mirizzi syndrome as it allows for the anatomical locations of the impacted gallstone and the common hepatic duct to be identified [9, 10]. Intraoperative cholangiography is useful for cases in which the identification of the common hepatic duct is difficult due to severe inflammation. In addition, after extracting the impacted gallstone, we could identify the common hepatic duct because the ENBD tube had already been placed into the lumen of the common hepatic duct. Thus, the insertion of an ENBD tube may be important for securing the safety of laparoscopic procedures to treat Mirizzi syndrome.
In conclusion, we experienced a case of Mirizzi syndrome Type II that was successfully treated by choledochoplasty using a gallbladder patch via a purely laparoscopic approach.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest in association with the present study.
FUNDING
None.
REFERENCES
- neck
- back pain
- endoscopic retrograde cholangiopancreatography
- endoscopy
- biliary calculi
- bile ducts
- intraoperative care
- laparoscopy
- nausea
- surgical procedures, operative
- sutures
- desire for food
- appetite or desire
- gallbladder
- surgery specialty
- laparoscopic surgery
- mirizzi's syndrome
- tube drain
- cholangiogram, intraoperative
- choledochoplasty
- filling defect
- hartmann's pouch
- gallbladder wall



