-
PDF
- Split View
-
Views
-
Cite
Cite
Mariko Tanaka, Toshiyasu Kawahara, Takahiro Nishikoshi, Masahiro Hagiwara, Koji Imai, Kimiharu Hasegawa, Atsuhiro Koya, Naoto Matsuno, Hidehiro Takei, Nobuyoshi Azuma, Hiroyuki Furukawa, Successful surgical treatment for huge retroperitoneal liposarcoma involving the pancreas, right kidney, abdominal aorta and inferior vena cava, Journal of Surgical Case Reports, Volume 2017, Issue 11, November 2017, rjx200, https://doi.org/10.1093/jscr/rjx200
Close - Share Icon Share
Abstract
Retroperitoneal liposarcoma is a rare neoplasm that often involves other organs and major blood vessels. Complete surgical resection with negative margins is the only potential curative treatment. Here, we report the case of a patient with a large retroperitoneum liposarcoma that was removed by resection of the descending abdominal aorta and infrahepatic inferior vena cava, right nephrectomy and pancreatoduodenectomy following creation of an extra anatomical femoro-femoral crossover bypass after left axillo-left femoral bypass. The patient developed leg edema for a few weeks after surgery but this condition was gradually resolved with diuretics. Otherwise, no serious postoperative complication was observed, and the patient was discharged at 37 days after surgery. There has been no evidence of recurrence for 16 months. In conclusion, radical surgical resection is a possible therapeutic option for retroperitoneal liposarcoma involving major vessels or other organs, and may improve survival if negative resection margins can be achieved.
INTRODUCTION
Retroperitoneal liposarcoma (RL) is a relatively rare neoplasm, complete surgical resection of the tumor with negative margins is the only way to achieve long-term survival [1, 2]. Some RLs involve major blood vessels as well as other organs, which might be a reason not to perform surgical resection. Here, we report the case of a large RL that was resected, including resection of the descending abdominal aorta and infrahepatic inferior vena cava (IVC), right nephrectomy and pancreatoduodenectomy following creation of an extra anatomical femoro-femoral crossover bypass after left axillo-left femoral bypass (Ax-F & F-F bypass).
CASE REPORT
A 60-year-old female visited a clinic because of abdominal distension. She noticed abdominal distention one year prior to her clinical visit, but she left it for a year. Gradual enlargement of the mass eventually made her decide to see a doctor. Enhanced abdominal computed tomography (CT) revealed large retroperitoneal tumors. Mini-laparotomy and tumor biopsy confirmed her diagnosis as dedifferentiated liposarcoma, then she was referred to us for further examination and treatment. A multidetector CT scan revealed a hypodense mass in the retroperitoneum, with a size of ~30 × 20 cm2. The tumor appeared to invade the duodenum, head of the pancreas, right kidney, IVC and abdominal aorta (Fig. 1). The IVC was almost occluded by the tumor, but venous return from the lower extremities beyond the tumor was observed through collateral veins around the tumor (Fig. 2). The tumor invaded the abdominal aorta just below the left renal artery to the common iliac artery bifurcation, although the root and entire length of SMA appeared to be free from the tumor (Fig. 3). She underwent en bloc resection of the RL with resection of the right kidney, duodenum, head of the pancreas, a portion of the inferior IVC and abdominal aorta. Ax-F & F-F bypass was performed for vascular reconstruction using poly-tertrafluoroethylene (PTFE) to maintain the blood flow to the both lower extremities (Fig. 4). The lower abdominal aorta and both sides of common iliac arteries were resected with the tumor. The proximal stump of the abdominal aorta was closed with a running suture and covered by the omentum. The IVC was resected from just below the left renal vein to the common iliac veins. Reconstruction of the venous system including IVC and common iliac veins was not performed because venous collateral pathways had already developed sufficiently. Child’s reconstruction was performed after pylorus-preserving pancreatoduodenectomy. The duration of the surgery was 19 h 22 min, and blood loss was 4 811 mL, requiring 1680 mL of red blood cell transfusion. The tumor was 33 × 20 × 13 cm3 in size, weighed 4800 g, and had a fibrous capsule (Figs 5 and 6). Pathological examination revealed a dedifferentiated liposarcoma with negative margin (Fig. 7). Tumor invaded the pancreatic capsule, the renal capsule, the adventitia of the IVC and the abdominal aorta and infiltrated into the muscularis propria and focally into lamina propria of the duodenum. Edema of the both lower extremities was noted as postoperative complication, but that was gradually resolved by diuretics. The patient was discharged 37 days after surgery without serious postoperative complications such as pancreatic fistula, as well as graft infection or obstruction of two bypasses. Currently, she remains alive and well with no evidence of recurrence at 16 months post-operation.
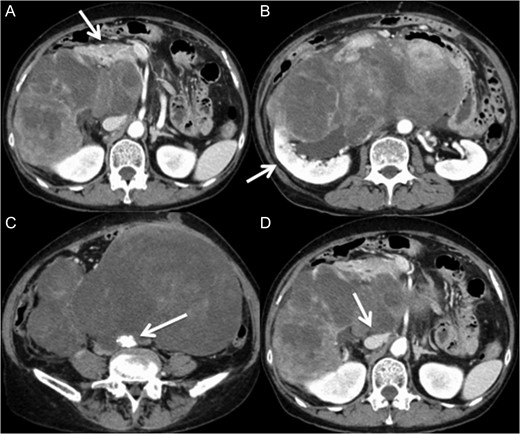
Multidetector CT scan (axial view). The large retroperitoneal tumor was adjacent to the duodenum, the head of the pancreas (A) and the right kidney (B). The tumor surrounded the abdominal aorta (C) and the inferior vena cava (D).

Multidetector CT scan (coronal view). The tumor invaded the IVC from the orifice of the right renal vein and the peripheral IVC was almost fully occluded.
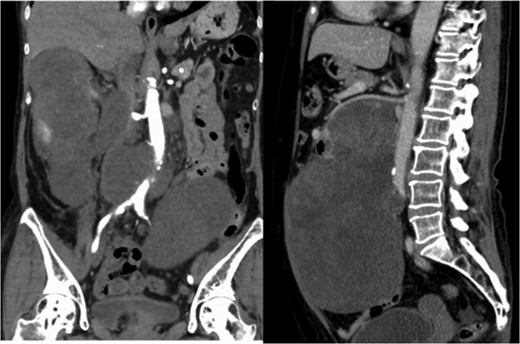
Multidetector CT scan (coronal view and sagittal view). The tumor surrounded the abdominal aorta from the superior mesenteric artery orifice to the common iliac artery bifurcation.

Mesenterium invasion of large retroperitoneal tumor. A huge tumor with a fibrous capsule invaded mesenterium, but SMA was free from the tumor.
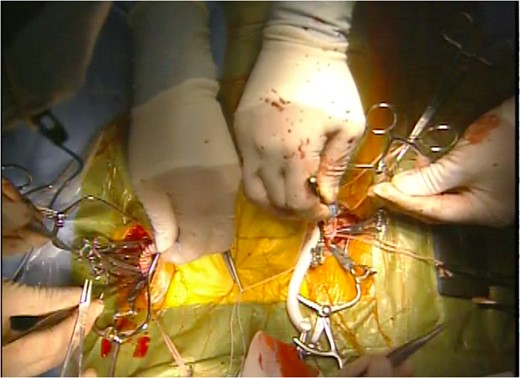
Anatomical femoro-femoral crossover bypass after left axillo-left femoral bypass. Ax-F & F-F bypass were performed for vascular reconstruction using poly-tertrafluoroethylene (PTFE) to maintain the blood flow to the both lower extremities
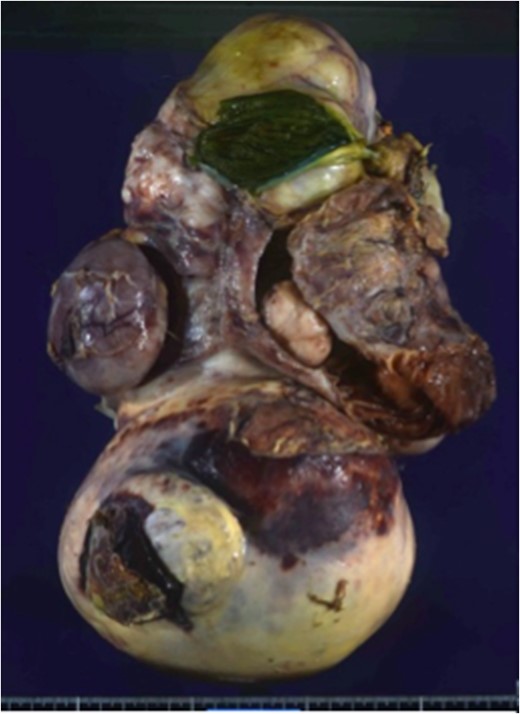
Macroscopic findings of the tumor. The resected specimen measured 33 × 20 × 13 cm3 and weighed 4800 g.
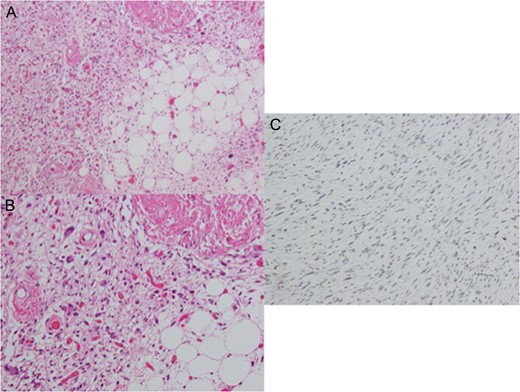
Microscopic findings of the tumor. Histopathological examination showed that the tumor was composed of a mixture of well-differentiated lipoblast and plemorphic liposarcoma with both atypical nuclear and multinuclear spindle cells. (A) Hematoxylin-eosin staining, ×10; (B) hematoxylin-eosin staining, ×20. Tumor cells were positive for MDM-2 ((C) imunohistochemistry of MDM-2, ×20). We diagnosed it as dedifferentiated liposarcoma.
DISCUSSION
RL is not often detected until it becomes enlarged because it does not demonstrate any characteristic symptoms. Chemotherapy has been established in the patients with advanced soft tissue sarcoma [3], the response rate was 25% in dedifferentiated liposarcoma [4]. Therefore, complete resection of the tumor with negative margins is recommended. Previous studies have shown that the histologic subtype and margin of resection are the most important prognostic factors for the survival of patients with RL [1, 2]. However, because it often involves other organs and major blood vessels, combined resection of those structures with RL is often required to achieve complete resection with negative margins. While a malignant epithelial tumor with major vascular invasion is not usually a candidate for surgery, sarcoma with major vascular invasion often become a good candidate. Matthias et al. reported that 25 patients with retroperitoneal sarcoma with vascular invasion successfully underwent en bloc resection of the tumor with the involvement of blood vessels. They concluded that complete resection with negative margins was important for long-term survival and that resection of the tumor en-bloc with major vascular systems is a potential treatment option when it involves major vascular structures [5]. The 5-year survival rates were 66.7%, after complete resection with tumor-free resection margins, although a poor outcome with 21-month median survival for patients who received complete resection with a positive resection margin was observed. There are several reports demonstrating that complete resection of vascular involvement improves the prognosis of patients with retroperitoneal sarcoma [6–8]. In our case, the tumor invaded the duodenum, head of the pancreas, right kidney, IVC and aorta. Therefore, removal and reconstruction of those involved organs and the surrounding vessels were necessary to achieve complete tumor resection. Reconstruction of the IVC was not performed because it was already occluded by the tumor and a collateral venous pathway had developed. We selected Ax-F & F-F bypass through the subcutaneous root for the reconstruction of the aorta to avoid vascular graft replacement infection because an intra-abdominal vascular graft has risks of infection associated with pancreatic fistula following pancreatoduodenectomy. Although Ax-F & F-F bypass is usually inferior to anatomical bypass with respect to patency, it has been reported that the 5-year patency rate of Ax-F & F-F bypass is 71% for peripheral arterial occlusive disease [9, 10], which seems acceptable. In this case, the patient had no serious postoperative complications. The graft patency was maintained, and there is no evidence of recurrence after 16 months.
In conclusion, extended tumor resection might be considered in patients with RL involving other organs and major vascular structures when complete resection with negative margins is possible. However, cautious consideration in regard with the surgical indication is necessary when the patient needs vascular reconstruction.
CONFLICT OF INTEREST STATEMENT
None declared.



