-
PDF
- Split View
-
Views
-
Cite
Cite
Shin-ichi Kosugi, Takehisa Hashimoto, Yo Sato, Kenichiro Hirano, Eiji Sunami, Takeaki Matsuzawa, Motoko Takahashi, Hiroshi Ichikawa, Cardiac tamponade communicating with a posterior mediastinal chylocele after esophagectomy, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx216, https://doi.org/10.1093/jscr/rjx216
Close - Share Icon Share
Abstract
A 75-year-old male received neoadjuvant chemotherapy for locally advanced squamous cell carcinoma of the mid-thoracic esophagus, followed by right transthoracic esophagectomy with extended mediastinal lymphadenectomy. Cardiac tamponade developed on postoperative Days 1 and 13, for which emergency ultrasound-guided drainage was required. Pericardial drainage fluid became chylous after administration of polymeric formula. A computed tomography scan demonstrated the presence of a retrocardiac fluid collection, encompassed by the left pulmonary vein and left atrium, descending aorta and vertebral column. Based on these findings, the diagnosis of chylopericardial tamponade communicating with a posterior mediastinal chylocele was made. The ligation of the thoracic duct was successfully performed via the left-sided thoracoscopic approach on postoperative Day 20 and the clinical course after the second operation was uneventful. The possible mechanisms of this exceptionally rare complication after esophagectomy were discussed.
INTRODUCTION
There have been two types of cardiac tamponade after esophagectomy reported in the literature so far. One is due to extrinsic compression of the heart, caused by the herniated colon [1], mediastinal chylocele [2] and dilated gastric tube [3]. This condition is mimicking typical cardiac tamponade and referred to as extrapericardial tamponade. Another is due to intrapericardial fluid collection, caused by postoperative bleeding [4] and acute pericarditis [5]. This condition is typical of cardiac tamponade; however, this type of complication is relatively scarce. There have been two reports of chylopericardium after esophagectomy that was probably caused by the interruption of lymphatic drainage from the heart and pericardium, due to postoperative radiotherapy [6] and ligation of the thoracic duct for postoperative chylothorax [7]. To the best of our knowledge, however, chylopericardial tamponade communicating with a posterior mediastinal chylocele after esophagectomy has not yet been reported.
CASE REPORT
A 75-year-old male received neoadjuvant chemotherapy for clinical T3N1M0 squamous cell carcinoma of the mid-thoracic esophagus according to the tumor-node-metastasis (TNM) classification of the International Union against Cancer (UICC), followed by right transthoracic esophagectomy with extended mediastinal lymphadenectomy. The thoracic duct, pericardium and left mediastinal pleura were partially resected due to suspected tumor invasion. Gastric tube was pulled up through the retrosternal route and anastomosed with the cervical esophagus. Finally, the tumor was staged as ypT3N1M0 with no chemotherapeutic effect by the histological examination of the resected specimen and R0 resection was achieved according to the UICC’s residual tumor classification. The patient had no intraoperative complications and was sent to an intensive care unit for early postoperative management.
Enteral feeding with low-fat elemental formula was commenced in the morning on postoperative Day (POD) 1; however, hemodynamic instability suddenly developed in the afternoon on the same day. Echocardiography performed during cardiopulmonary resuscitation demonstrated massive pericardial effusion. Emergency ultrasound-guided drainage was performed via the subxyphoid approach; 350 mL of serous fluid was drained, and the patient’s hemodynamic status dramatically improved. After changing to fat-containing polymeric formula on POD 5, a small amount of chylous fluid was contained in the pericardial drainage fluid, but not in the bilateral pleural drainage fluid. Because the chylous fluid disappeared immediately after returning to the elemental formula, the right pleural, pericardial, and left pleural drains were removed sequentially. A fat-reduced diet was given to the patient; however, the cardiac tamponade relapsed and the pericardial drain was re-inserted on POD 13. A computed tomography scan demonstrated the presence of a retrocardiac fluid collection, encompassed by the left pulmonary vein and left atrium, descending aorta and vertebral column (Fig. 1). The initial pericardial drainage fluid was serous, but it changed to chylous again after a challenge with polymeric formula. Under the diagnosis of chylopericardial tamponade communicating with a posterior mediastinal chylocele, surgical exploration was performed via the left-sided thoracoscopic approach on POD 20. A chyle leak from a tributary of the thoracic duct was easily recognized because of the administration of polymeric formula immediately before surgery. The leak was stopped with surgical clips. A pericardial hole, which had been made during the esophagectomy, was confirmed to be close to the leakage point (Fig. 2). The hole was left open and a closed suction drain was placed in the posterior mediastinum.
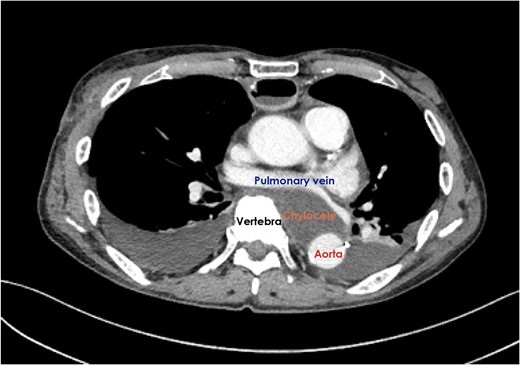
Computed tomography scan demonstrated the presence of a retrocardiac fluid collection when the cardiac tamponade relapsed.
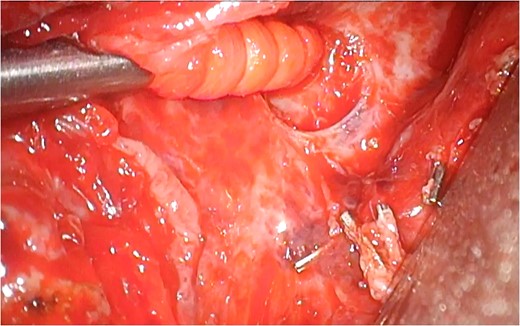
A pericardial hole was confirmed to be close to the leakage point.
The clinical course after the second operation was uneventful, with neither the cardiac tamponade nor the chyle leakage relapsing after the resumption of a regular diet. The patient was discharged home on POD 38 after the esophagectomy.
DISCUSSION
The anatomical characteristics of this patient should be considered when discussing the development of this exceptionally rare complication. As shown in Fig. 1, the descending aorta was located dorsally in the left thoracic cavity; therefore, a space was encompassed by the left pulmonary vein and atrium, descending aorta and vertebral column. A bulky esophageal tumor occupied this space before the operation, while a chylocele replaced the tumor after it was removed. As reported by Rottoli et al. [2], chylous fluid would usually drain into the right thoracic cavity, even if a chylocele developed in the posterior mediastinum. Interestingly, vertebral column prevented chylous fluid from draining into the right thoracic cavity in this patient; therefore, no chyle drainage from the right chest tube was seen throughout the clinical course. Moreover, no chylous fluid drained into the left thoracic cavity either, although the left mediastinal pleura was partially resected with tumor of the mid-thoracic esophagus at the initial operation. The second operation revealed that the opened pleura was already covered by the left lung, which tightly adhered to the descending aorta. Because of this completely isolated space, increased chylous fluid would flow into the hypobaric pericardial space through a small hole in the pericardium.
There is no definite opinion about how to manage the pericardial hole occurring during esophagectomy. No problem usually occurs if the hole is left open. It was uncertain whether wide excision of the pericardium could prevent the cardiac tamponade in this case. Wide excision of the pericardium would form the pericardial space and posterior mediastinum into one component. As long as chylous fluid from the thoracic duct would continuously flow into this component, cardiac tamponade might develop irrespective of the size of the pericardial defect. On the other hand, primary closure is usually unnecessary because cardiac herniation is less likely to occur through the hole, which is covered with vertebral column. Considering the particular condition of this patient; however, primary closure might be preferable to wide excision and could prevent the cardiac tamponade in this case.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- pericardial sac
- cardiac tamponade
- ultrasonography
- left atrium
- computed tomography
- descending aorta
- squamous cell carcinoma
- esophagectomy
- lymph node excision
- polymers
- pulmonary veins
- thoracoscopy
- diagnosis
- esophagus
- mediastinum
- spine
- lymph node dissection
- thoracic duct ligation
- esophagectomy by abdominal and transthoracic mobilization
- chemotherapy, neoadjuvant



