-
PDF
- Split View
-
Views
-
Cite
Cite
Dilasma Ghartimagar, Ujjwal Koirala, Arnab Ghosh, Manish Kiran Shrestha, Sushma Thapa, Raghavan Narasimhan, O.P. Talwar, Squamous cell carcinoma arising in familial gingival fibromatosis—a rare case report, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx197, https://doi.org/10.1093/jscr/rjx197
Close - Share Icon Share
Abstract
Familial gingival fibromatosis is a rare hereditary condition due to chromosomal abnormality which can occur as an isolated disease or as part of a syndrome and has an incidence of 1:350 000. This condition leads to esthetic, functional, psychological and masticatory disturbance of the oral cavity. Here, we present a case of 21-year-old female with severe enlargement of gums in maxilla and mandible. Deciduous teeth were erupted at normal age but the permanent teeth in the oral cavity were not erupted. Her grandmother, father and younger sister were also affected with the same condition. Incisional biopsy from the chronic ulcerated gingiva showed squamous cell carcinoma. Patient was referred to other cancer institution, where metastases to lung, bone and lymph node was detected on CT scan. The diagnosis was made based on clinical examination, family history and histopathological examination.
INTRODUCTION
Familial gingival fibromatosis (FGF), also known as elephantiasis gingivae is a rare hereditary condition with an incidence of 1: 350 000. The condition leads to esthetic and functional abnormality of oral cavity and even psychological disturbance [1, 2]. It occurs due to chromosomal abnormality. It is characterized by overgrowth of gingival tissue [2].
CASE REPORT
A 21-year-old female presented with marked swelling in her gums for approximately past 13 years which recently increased in size. She also complained of difficulty in mastication and speech. On examination, there was extensive gingival hypertrophy involving both upper and lower jaws. Extensive areas of surface ulceration with pus collection were noted (Fig. 1). There was no eruption of permanent teeth. She had mental retardation but her physical growth was normal.

Patient presented with marked swelling of her gums with extensive areas of surface ulceration and pus collection.
Patient said that deciduous teeth were normal but after falling off of deciduous teeth, permanent teeth did not erupt and gum enlargement started progressively. She studied only up to second Standard in school after which she dropped out due to this condition.
On inquiry, she said that her grandmother, father and younger sister also have similar condition. She has two brothers who do not have this condition.
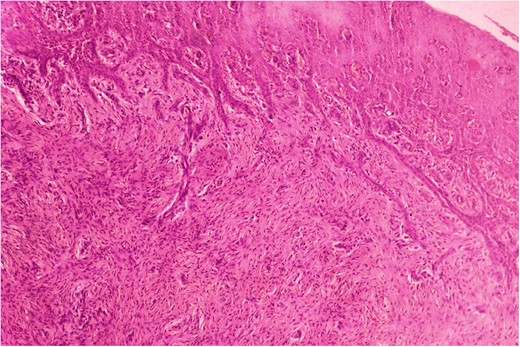
Biopsy was taken from hypertrophied and ulcerated lesion. On microscopy, tissue was lined by keratinized stratified squamous epithelium with surface ulceration. Underlying stroma showed infiltrating squamous cell carcinoma (SCC) along with extensive collagenous fibrosis (Fig. 2). Dense acute and chronic inflammations were also noted. A diagnosis of SCC with familial gingival fibromatosis was given (Fig. 3).
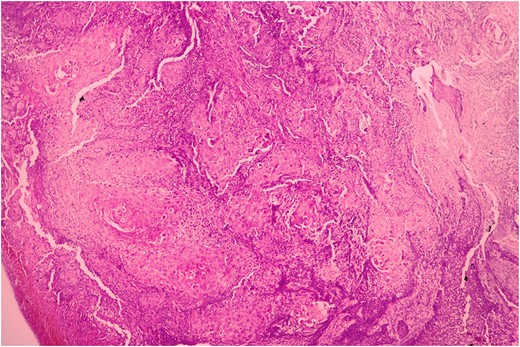
Histopathological picture showing islands of squamous cell carcinoma infiltrating into the stroma. (H&E, ×400).
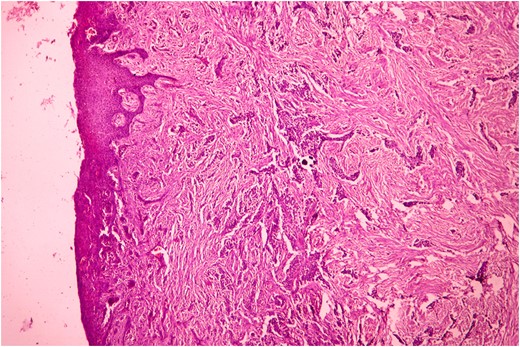
Histopathological picture showing infiltrating squamous cell carcinoma along with bundles of collagenous fibrous connective tissue. (H&E, ×400).
Patient was referred to cancer institution, where metastases to cervical lymph nodes, lung and bone were detected on CT scan. Patient and her family were unwilling to go for further treatment due to financial condition and subsequently she passed away after 14 months of initial presentation.
Her younger sister with age 17 years also presented 4 months later with similar complaints (Fig. 4). She also had normal deciduous teeth but did not have any permanent teeth eruption. She had difficulty in mastication and speech as well. She was mentally sound and did not have any other abnormalities. All her routine investigations were normal. X-ray (Fig. 5) and CT (Fig. 6) scan showed permanent teeth in both upper and lower arch which were malpositioned, unerupted and impacted in fibrous growth. Biopsy was taken from the gingival growth of younger sister which showed stratified squamous lining and subepithelial tissue showed collagenous fibrous connective tissue with mild chronic inflammatory cells (Fig. 7). Diagnosis of FGF was given. She underwent two stage gingivectomy 2 weeks after the initial diagnosis of FGF (Fig. 8). She is doing well and able to close her lips on post-operative follow-up (Fig. 9A). Later, prosthetic rehabilitation was done with upper and lower complete removable denture to the younger sister (Fig. 9B).
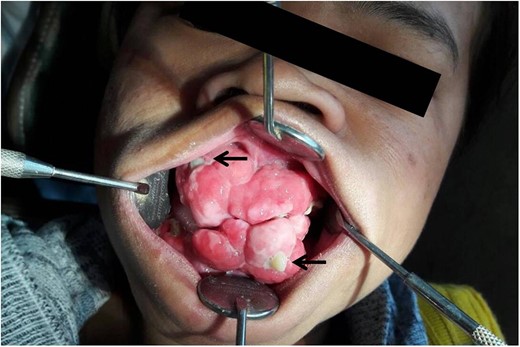
Younger sister of the patient presenting with swelling of her gums and impacted teeth (black arrow) in fibrous growth.

X-ray picture of younger sister showing impacted and malpositioned permanent teeth in upper and lower arch.
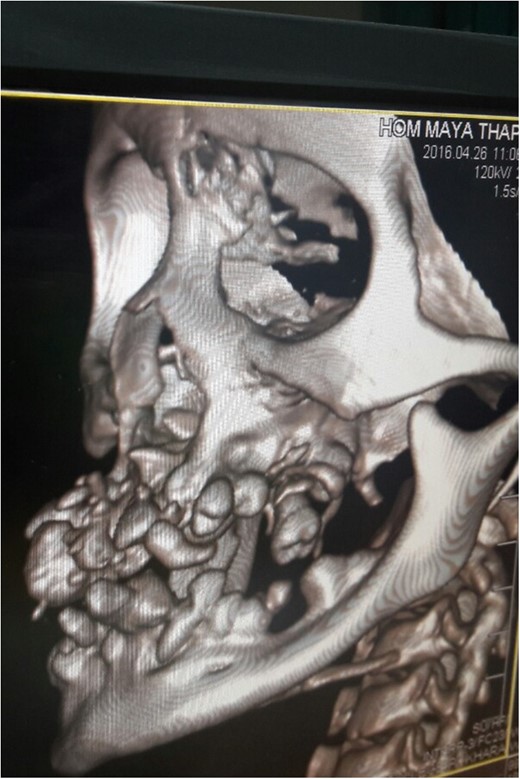
CT scan of younger sister showing permanent teeth in both upper and lower arch which are malpositioned and unerrupted and impacted.
Histopathological picture of younger sister showing stratified squamous lining and subepithelium shows rich collagenous fibrous connective tissue with mild inflammatory cells. (H&E, ×400).


Post-operative picture after 3 months (A) and prosthetic rehabilitation with upper and lower complete removable denture of younger sister on follow-up after 6 months (B).
Her father aged 52 years who had similar condition for more than 40 years had recent increase of gingival swelling along with ulceration and pus collection (Fig. 10). He went to the same cancer institution, where clinically malignancy was suspected and biopsy was taken. He passed away within 10 days of biopsy. The biopsy showed infiltrating SCC.

Patient’s father presenting with swelling of his gum with areas of surface ulceration and pus collection.
DISCUSSION
Gingival fibromatosis is familial/idiopathic and is usually inherited as autosomal dominant trait or less commonly as autosomal recessive. FGF may manifest as an isolated disorder or part of a syndrome. The familial form may occur with a number of other inherited syndromes, e.g. Zimmerman Laband Syndrome, Murray Puretic Drescher, Rutherfurd Cross Cowden Syndrome, Tuberous sclerosis [2–4]. Here, we report a case of an isolated FGF as it did not show other associated signs and symptoms relating to any syndromes.
FGF is characterized by diffuse enlargement of gingiva that is slowly progressive covering partly or total tooth surface. The gingival overgrowth is due to excessive production of collagen in gingiva which usually does not affect the alveolar bone [5]. The gingival hyperplasia can be generalized (symmetric) or localized (nodular) [5].
FGF is seldom present at birth. It usually begins at the time of permanent dentition. It may interfere with or prevent the eruption of permanent teeth as in our case [6]. FGF has been genetically linked to chromosomes 2p21-p22 and 5q13-q22. Recently mutation in SOS-1 gene has been suggested as a possible cause [2]. The fibroblasts are permanently activated due to TGF-beta and grow faster and produce more collagen and fibronectin than normal fibroblasts. Elevated expression of protoconcogence c-myc is suggested for deregulated cell growth [3, 7].
Histopathologically, the bulbous increased connective tissue is relatively avascular and shows densely arranged collagen bundles, numerous fibroblasts and chronic inflammatory cells. The overlying epithelium is usually acanthotic and has elongated rete ridges [8].
Clinically, the FGF is often associated with hypertricosis, growth retardation, mental deficiency, corneal dystrophy, nail defects, deafness and craniofacial deformities. In our case, only mental retardation was noted in the elder sister while her father and younger sister were normal.
In our report, the elder sister and her father both had the condition for many years which led to ulceration and subsequently infiltrating SCC. SCC is the commonest malignant neoplasm affecting structures of the oral mucosa and accounts for more than 90% of all malignant lesions in the mouth. The most common sites includes tongue and floor of mouth followed by the soft palate, gingiva and buccal mucosa [9].
Treatment varies according to the degree of severity. In severe cases, series of gingevectomies with maintenance of oral hygiene is required [2]. In our case also, two stage gingevectomy was performed for the younger sister and she is doing well till date. Recurrence is common after surgery and close follow-up is necessary. There is debate regarding the correct time of surgery. Eruption of complete set of permanent teeth normally occurs at the age of 12 years which is the recommended time for surgery [10].
FGF is a rare but an important hereditary disorder. Our report outlines the details of a single family experience and the malignant transformation in two family members. We highlight that transformation can happen at a very early age when compared to the population unaffected by Familial Gingival Fibromatosis.
ACKNOWLEDGEMENT
None.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
REFERENCES
- computed tomography
- chromosome abnormality
- cancer
- squamous cell carcinoma
- chromosomal disorder
- physical examination
- ulcer
- permanent tooth
- esthetics
- father
- gingival fibromatosis
- gingiva
- maxilla
- mouth
- deciduous tooth
- diagnosis
- hypertrophy
- lymph nodes
- mandible
- metastasis to the lung
- incisional biopsy
- histopathology tests
- grandmother



