-
PDF
- Split View
-
Views
-
Cite
Cite
Françoise Schmitt, Philippe Topart, Agnès Salle, Loïc Sentilhes, Natacha Bouhours-Nouet, Régis Coutant, Dominique Weil, Guillaume Podevin, Early postpartum gastric band slippage after bariatric surgery in an adolescent obese girl, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw155, https://doi.org/10.1093/jscr/rjw155
Close - Share Icon Share
Abstract
We report here a case of a rarely described complication of laparoscopic adjustable gastric banding (LAGB), slippage during the postpartum period, after LAGB had been performed in an adolescent obese girl. The LAGB had been placed after one year of clinical survey initiated at the age of 16. Maximal pre-operative body mass index (BMI) was 48.5 kg.m−2 and obesity was associated with insulin resistance. Before pregnancy, there was a loss of 17 Kg (final BMI = 41.5 kg.m−2) and a resolution of insulin resistance. The patient became pregnant 21 months after LAGB, and whole pregnancy and delivery were uneventful for both mother and fetus. Six weeks after delivery, the patient suddenly complained for total food intolerance, due to a band slippage, leading to removal of the band. Slippage is now a rare complication of LAGB, but can happen during pregnancy and the postpartum period as well.
Introduction
In Europe, up to 50% of women of reproductive age and 20–25% of pregnant women at the first antenatal visit are overweight or obese. Obese mothers display higher frequencies of morbidities and mortality [1], and their offspring shows higher frequencies of stillbirth, neonatal death, congenital anomalies and macrosomia [2]. Nowadays, almost half of all patients who undergo bariatric surgery are or will be women of reproductive age. Studies on the effects of bariatric surgery on pregnancy suggest that obstetrical and neonatal outcomes are improved [3], but generally focus on maternal and fetal outcomes [4] and seldom report occurrence of surgical complications during pregnancy. We report here an acute gastric prolapse through the band during the postpartum period in a post-adolescent woman, which has fast never been described herein.
Case report
This case report has been extracted from the prospective survey of the cohort of adolescents undergoing bariatric surgery in our specialized care center. This cohort has obtained institutional review board approval in 2008 and patients gave their informed consent.
The efficacy of LAGB on weight loss and on obesity-associated comorbidities was assessed as previously described [5].
The clinical course of the patient began in our specialized care center at the age of 16. She weighed 116 kg, corresponding to an initial BMI of 45.9 kg.m−2. Her obesity was associated with insulin resistance (HOMA-IR = 3.87, z-score for fasting insulinemia = +2.41 standard deviation (SD)), and low high-density lipoprotein (HDL) cholesterol at 0.82 mmol/l (−2.85 SD). One year later, in spite of dietary and medical assistance, she weighed 122 kg and had a BMI of 48.5 kg m−2. The LAGB was then placed laparoscopically, using the ‘pars flaccida’ method, and the band was fixed to the stomach. The whole procedure and early postoperative period were uneventful. Within 18 months after LAGB, there was a loss of 17 kg (final BMI = 41.5 kg m−2) corresponding to a 28% of excess body weight loss, and a resolution of insulin resistance (HOMA-IR = 1.85, z-score for fasting insulinemia = +1.98 SD). HDL cholesterol remained at the previous values (0.77 mmol/l).
The patient became pregnant 21 months after LAGB. A monthly specialized survey was done, including systematic screening for trace metal and vitamin deficiencies. Adequate supplementation in vitamins B6, B9, B12, D, folate, magnesium and iron was provided. There was no complication of pregnancy, such as gestational diabetes mellitus, gestational hypertension nor preeclampsia, and fetal growth parameters remained within the normal range. The LAGB was kept inflated (5 ml) during the whole pregnancy, and final weight gain was 1.7 kg. Delivery of a 3,100 g male newborn occurred at 39 + 5 weeks of gestation by spontaneous vaginal delivery. Six weeks after delivery, the patient suddenly complained for total food intolerance and vomiting. Contrast meal showed an anterior band slippage, with partial stoma occlusion (Fig. 1). The LAGB could not be simply deflated and required revision, but the patient preferred to definitely remove the band, which was done under laparoscopy without surgical complication.
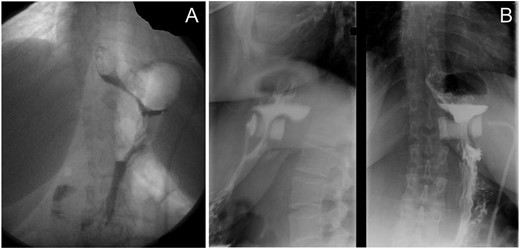
Contrast meal before and after pregnancy. (A) The band in good place 1 month before the beginning of pregnancy with good emptying of the gastric pouch. (B) The anterior band slippage with incomplete superior gastric pouch occlusion, 6 weeks after delivery.
Discussion
We report here the first case of band slippage that occurred during the postpartum period in a young woman who had a LAGB placed as she was still adolescent. To our knowledge, there are yet no studies dealing with the effects of adolescent bariatric surgery on later pregnancies. Complications related to LAGB during pregnancy have been explored in many series and reviews [3, 4, 6], mainly dealing with complications related to fetal and maternal outcomes but only reporting few surgical complications of the band. Hence, a recent review of Vrebosch et al. [6] on 728 pregnancies in 638 women having an LAGB only reports nine band slips (1.2%), three band disconnections, two band migrations and two port leaks during pregnancy and eight (1.1%) LAGB slippages during the postpartum period. The most reported interventions on the band are adjustments for fear of vomiting or risk of nutrient deficiencies for the fetus, habits of the surgical team or hyperemesis gravidarum [7, 8].
Anatomical changes during pregnancy include horizontalization and elevation of the stomach, which may cause displacement of the band or favor proximal pouch dilation [9]. Nevertheless, pregnancy does not seem to increase the risk of band slips, as the recently reported rate of 2.3% of band slips around pregnancy [6] remains comparable to the 2–10% rate reported in the non-pregnant LAGB population [10]. However, the study of Haward et al. [9] reported trends toward more proximal pouch dilations including band slips during the 3 years after pregnancy, suggesting an effect of the later on band-related complications. Specific reports of LAGB slippage during the postpartum period are scarce, and the only series is one of Carelli et al. [7] reporting up to 6.7% of LAGB slippages within 6 months after childbirth. An adequately filled band during pregnancy has not been identified as a risk factor for peripartum band slips, and most teams only adjusts bands if clinically required during pregnancy [7], to prevent excessive maternal weight [8]. In our case, we maintained the band filled as the patient did not present vomiting during her pregnancy, and the symptoms only began 6 weeks after delivery, indicating that intra-abdominal anatomical changes after pregnancy may play a role in band complications too. She became pregnant 21 months after LAGB placement, which could be a risk factor for band slips, according to the study of Haward et al [9], which demonstrated that there were less band revisions if the pregnancy occurred >2 years after bariatric surgery.
In conclusion, this case report emphasizes the fact that band slip can occur during pregnancy, and the postpartum period may be due to quick anatomical maternal changes but not with a higher frequency than usually reported. Patient counseling should integrate this topic, with particular regards toward the delay before conception and the band adjustment principles during pregnancy.
Conflict of interest statement
None declared.



